
And the Hepatocellular Carcinoma Goes to… Masseter!
*Corresponding Author(s):
Elsa Amorim SilvaDepartment Of General Surgery, Hospital Of Braga, Braga, Portugal
Tel:+351 253080800,
Email:elsaamorimsilva@gmail.com
Abstract
Hepatocellular carcinoma is the most frequent primary malignant tumor of the liver. Disease dissemination frequently involves the bone, adrenal glands, pancreas and lungs. Other soft tissue metastasis are extremely rare.
A 71-year-old male patient with a history of chronic alcoholism was diagnosed with hepatocellular carcinoma (cT1N0M0) at September, 2010 and a partial hepatectomy (subsegmentectomy V/VI) was performed (pT3a G2 Nx). At that time, the patient referred a left preauricular painless nodule. Due to nonspecific features on ultrasonographic evaluation and absence of lymphadenopathies, the nodule was considered to be benign and no further investigation was done.
Thirty months after initial surgery, the patient presented with a significantly increased nodule on left masseter. The biopsy showed a hepatocellular carcinoma metastasis and a surgical excision was performed.
The case we present is a very rare example of metastatic HCC involving rare locations without affection of the common ones.
This case seems to justify more efforts in the treatment of HCC even with single distant metastasis.
INTRODUCTION
CASE PRESENTATION
A 71-year-old male affected by chronic alcoholism presented with malaise and abdominal pain at the urgency hospital with an HCC suspected on Computed Tomography (CT) scan.
A liver biopsy was performed and confirmed the HCC diagnosis.
At that time the patient also presented a small mass in the left parotid region. The ultrasonographic evaluation showed a solid heterogeneous nodular lesion with 30x17x25mm embedded in the left masseter muscle, posteriorly to the parotid gland. There was no lymphadenopathies and the lesion was clinically interpreted as benign - Figure 1.
Figure 1: Cervical ultrasonography revealed a solid heterogeneous lesion with dimensions of 30x17x25mm located posteriorly to the left parotid gland.
The patient underwent a partial hepatectomy (subsegmentectomy V/VI) and cholecystectomy at October, 2010 (pT3a G2 Nx) - Figure 2.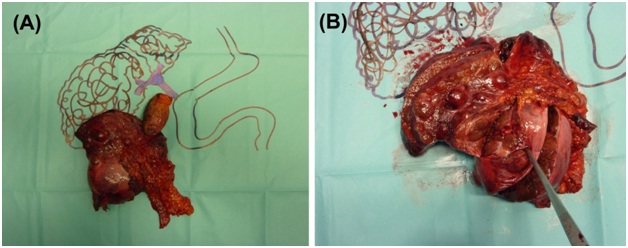
Figure 2: Macroscopic imaging of hepatic subsegmentectomy V / VI (14x9 cm) (A) Schematic drawing (B) HCC on the specimen.
A year later (October, 2011), the patient remained asymptomatic and performed a routine abdominal CT which showed a pericentimetric nodular lesion in the right hepatic lobe (segment V). An ultrasound guided alcoholisation was conducted in March, 2012.
At April, 2013 the patient mentioned a significantly increased on the left masseter nodule dimensions during the previous three months.
CT and Magnetic Resonance Imaging (MRI) showed a well-defined oval mass with 6 cm with necrotic center on the left cervical region - Figure 3. The lesion misplaced the parotid gland and there was no apparent cleavage plane with the masseter muscle and no bone invasion.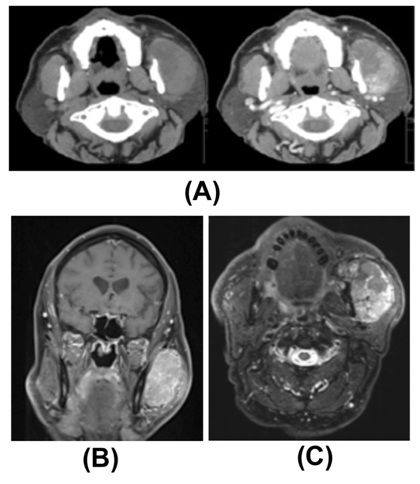
Figure 3: TC and Maxillofacial MRI showed extensive injury with oval configuration and necrotic content on the left cervical region without apparent cleavage plane with the masseter muscle (A) CT axial section (B) MRI coronal (C) MRI axial section.
The mass biopsy revealed a HCC metastasis.
A Positron Emission Tomography (PET) scan was also performed and it excluded other lesions suspicious of metastasis.
In multidisciplinary consultation it was decided to perform a surgical excision of the metastasis approached by otorhinolaryngology with neurophysiological monitoring of the facial nerve - Figure 4.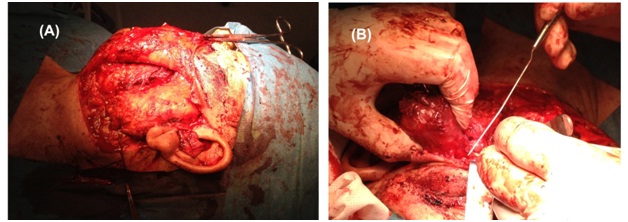
Figure 4: Surgical excision of masseter metastasis (A) Left parotid gland exposure, (B) Masseter metastasis.
Pathological examination of the surgical specimen confirmed previous diagnosis and the neoplasia was staged as pT3aG2N0M1 - Figures 5,6. Cirrhosis was also observed in the adjacent hepatic parenchyma.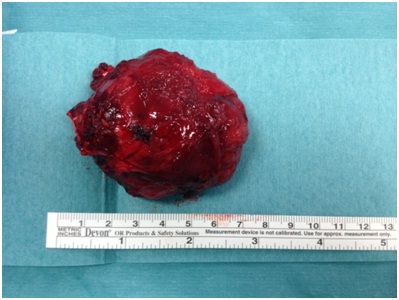
Figure 5: Macroscopic aspect of the excised masseter metastasis.
Figure 6: (A) Histological examination showed an infiltration of the masseter muscle by a metastatic hepatocellular carcinoma with pseudoglandular and trabecular pattern (H&E, 40x). (B) The tumour was composed by large eosinophilic cells with pronounced nuclear irregularity and hyperchomatism, very prominent nucleoli and cytoplasmic hyalineglobules (H&E, 400x). (C) The tumour cells showed strong cytoplasmic expression for hepatocyte specific antigen (400x). (D) Cancer cell emboli were observed in lymphaticvessels (H&E, 100x).
The patient was proposed to adjuvant radiotherapy and thereafter sorafenib.
The patient completed adjuvant radiotherapy (60Gy to the operated area) in December, 2013. A year later (December, 2014) it was suspended sorafenib because of cardiac toxicity (atrial fibrillation grade 2), cheilitis (grade 3), diarrhea (grade 2) and plantar erythrodysesthesia syndrome (grade 3) according to CTCAE (Common Terminology Criteria for Adverse Events, 2010).
The patient keeps follow-up in consultation and there is no evidence of recurrence to October, 2014.
DISCUSSION
Hepatocellular Carcinoma (HCC) spreads through hematogenous or lymphatic route and also by direct invasion into adjacent organs [1].
Extra hepatic metastasis of HCC were once regarded as a terminal event [2].
The most common sites of extra hepatic HCC are the lung, abdominal lymph nodes and bone. Incidental extra hepatic lesions seen by CT scan at less common sites, in patients with HCC who do not have metastatic disease at the more common sites, are unlikely to represent metastatic HCC [3].
The clinical course for patients with extra hepatic metastasis has not yet been completely elucidated. Some studies estimate the median survival after diagnosis of extra hepatic metastasis around 8.1 months. The cumulative survival rates at 1 year and 3 years were 48.9% and 10.6% if treatment were provided for extra hepatic metastasis [4].
Metastatic tumours of the masseter muscle are rare but diverse [5-7].
Solitary metastasis to the masseter in the setting of HCC is an exceptional phenomenon.
To the best of our knowledge, there is only one similar case reported in the literature referred to a HIV/HCV coinfected patient [8].
Few cases of parotid and mandibular metastasis have been described [9,10].
This case alerts to the fact that, inspite extra hepatic tumours at uncommon sites are unlikely to represent metastatic HCC, clinicians should be aware of that possibility.
Furthermore, the survival of this example case reinforces the importance of an accurate primary surgical management even in primary tumours of more advanced stages and with single metastasis.
REFERENCES
- Hong SS, Kim TK, Sung KB, Kim PN, Ha HK, et al. (2003) Extrahepatic spread of hepatocellular carcinoma: a pictorial review. Eur Radiol 13: 874-882.
- Bruix J, Sherman M, Practice Guidelines Committee, American Association for the Study of Liver Diseases (2005) Management of hepatocellular carcinoma. Hepatology 42: 1208-1236.
- Katyal S, Oliver JH 3rd, Peterson MS, Ferris JV, Carr BS, et al. (2000) Extrahepatic Metastases of Hepatocellular Carcinoma. Radiology 216: 698-703.
- Uchino K, Tateishi R, Shiina S, Kanda M, Masuzaki R (2011) Hepatocellular carcinoma with extrahepatic metastasis: clinical features and prognostic factors. Cancer 117: 4475-4483.
- Wong BJ, Passy V, DiSaia P (1995) Metastatic small cell carcinoma to the masseter muscle originating from the uterine cervix. Ear Nose Throat J 74: 118-121.
- Baude Brogniez A, Ferri J, Vandenhaute B, Lecomte Houcke M, Donazzan M (1997) Intra-masseter metastasis of a gastric adenocarcinoma. Rev Stomatol Chir Maxillofac 98: 303-305.
- Nakagawa H, Mizukami Y, Kimura H, Watanabe Y, Kuwayama N (1996) Metastatic masseter muscle tumour: a report of a case. J Laryngol Otol 110: 172-174.
- Berretta M, Zanet E, Di Benedetto F, Simonelli C, Bearz A, et al. (2008) Unusual presentation of metastatic hepatocellular carcinoma in an HIV/HCV coinfected patient: case report and review of the literature. Tumori 94: 589-591.
- Yu S, Estess A, Harris W, Dillon J (2012) A rare occurrence of hepatocellular carcinoma metastasis to the mandible: report of a case and review of the literature. J Oral Maxillofac Surg. 70: 1219-1223.
- Yu YD, Kim DS, Jung SW, Lee JH, Chae YS, et al. (2013) Metastatic hepatocellular carcinoma to the parotid gland: Case report and review of the literature. Int J Surg Case Rep 4: 76-78.
Citation: Silva EA, Freitas D, Cruz M, Moreira F, Babo A, et al. (2016) And the Hepatocellular Carcinoma Goes to… Masseter! J Clin Stud Med Case Rep 3: 034.
Copyright: © 2016 Elsa Amorim Silva, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

