Transmastoid Cartilage Graft-Meningocele Temporal: Surgical Approach
*Corresponding Author(s):
Mariana DC ToroDepartment Of Ear Nose Throat And Head And Neck Surgery, University Of Campinas, São Paulo, Brazil
Tel:+55 1935217523,
Fax:+55 1935217563
Email:mdctoro@gmail.com
Abstract
Introduction
Meningocele of the temporal bone is a herniation of meninges located in the middle ear, mastoid, petrous apex, or posterior fossa. The pathogenesis of this disease is a combination of temporal bone defects, along with a duramater alteration. Some correction techniques are described in the literature, but there is no consensus on the best approach.
Objective
The aim of this study is to describe the surgical treatment of temporal meningocele and to review the medical literature on this topic.
Methods
Retrospective analysis of clinical records of two patients who underwent surgical treatment for temporal bone meningocele along with review of the medical literature in PubMed.
Results
Both patients underwent surgical repair of meningocele via mastoidectomy with ear cartilage graft, fibrin glue and temporal fascia.
Discussion
In the literature, eight publications reporting 135 cases of meningocele of the temporal bone were found. Transmastoid and combined access with craniotomy surgical approaches were reported. The use of cartilage graft, temporalis fascia and mucosal flap closure for the correction of meningocele was described.
Conclusion
Meningocele temporal bone is a condition that must be considered as a differential diagnosis of otorrhea in patients with a history of ear surgery or trauma. Surgical correction is necessary for improvement of symptoms and prevention of meningitis. The technique described in this study proved effective for correction of pathology, which can be confirmed by similar results reported in the literature.
Keywords
INTRODUCTION
It can be divided in two groups according to the etiology: spontaneous or acquired. The most common kind is acquired, usually resulting from otologic infections, neoplasia, otologic surgery or head trauma. Spontaneous meningoencephalocele may occur mostly in the epitympanum or mastoid antrum and it can also be a result of pathologic obesity [2].
The pathogenesis of this disease results from a combination of bone defects along with an alteration of the duramater, that allows the herniation of brain and meningeal tissue, which explains why the bone defect itself is not sufficient to cause the meningocele [2]. Other factors that influents are alterations in the brain and meningeal tissue as edema, cysts and hemorrhage, pressuring the herniation through the bone defect [3].
Often it can be misdiagnosed because there are only few characteristic symptoms. The most expected symptoms are: unilateral conductive hearing loss with middle (secondary to reduce ossicular mobility), ear effusion on at patients older than 40 years-old, headache, pulsatile tinnitus or cerebrospinal fluid leak [4], those symptoms must be specially alarming if patient underwent recent trauma or surgery. It can also be presented with recurrent episodes of meningitis, and rarely associated with epilepsy of the temporal lobe [3].
The diagnosis of the disease must consider the symptoms and signs numerated above combined with otoscopy, in which fluid transparent liquid can be found along with signs of accentuated convexity of the tympanic membrane, particularly of the pars flaccida. However, the colorless characteristic of the fluid can lead to a normal otoscopy diagnosis in most of the cases. An audiometry may also show a unilateral conductive hearing loss [4].
The gold standard for temporal meningocele and temporal bone defects diagnosis and treatment is the high-resolution tomography. MRI can be useful if encephalocele is established for planning reduction of brain mass. Other studies such as cisthernography and nuclear medicine studies are more invasive, due to lumbar puncture, and they do not change diagnoses or therapy compared with CT. β2-transferrin tests can be done in cases of difficult diagnosis [4].
Temporal meningocele is an important pathology in otology and neurology practice for which surgery is required often. Closure of the defect can avoid meningitis, a potentially severe complication. In the other side, surgery has very few rates of complications [3].
The aim of this study is to describe the surgical approach of temporal meningocele and perform a medical literature review of this topic.
MATERIALS AND METHODS
Besides, a review of the medical literature in PubMed and Scopus database was performed, covering articles published since 1980 in Portuguese or English, using the following keywords (MeSH): “temporal bone meningocele, middle ear meningocele; hearing loss”. The aim of this review was to identify the surgical techniques most commonly used for the treatment of this pathology and its clinical outcomes.
Inclusion and exclusion criteria
The medical records of the subjects were used in this review and detailed all the parameters of the surgical procedure and related devices.
Ethics
RESULTS
Case 1
Case 2
Intra operative findings and surgical approach showed no temporal bone fracture line and it was performed a modified radical mastoidectomy, canal up surgery, and all ossicular chain and tympanic membrane were preserved.
Surgical approach
The operative field is prepared by ample trichotomy, antisepsis with 2% chlorhexidine, and placement of electrodes for monitoring the 8th cranial nerve. The operative field is separated from the rest of the scalp by using microporeTM. Antibiotic prophylaxis is done with endovenous cefazolin (50 mg/kg) during induction of anesthesia.
- Antisepsis with 0.2% aqueous chlorhexidine, placement of sterile drapes and steri-drape;
- Rectilinear retroauricular incision and dissection along anatomical planes.
- Removal of small fragments of fascia and temporal muscle;
- Resection of conchal cartilage.
- Simple mastoidectomy, identifying the lateral semicircular canal, the short ramus of the incus, the posterior wall of the outer ear canal, the tegmen timpani, and the lateral sinus;
- Dissection of the tegmen and visualization of the meningocele.
- Temporal muscle, cartilage and fascia along with fibrin glue is located. No other support was used.
- Closure with sutures on by planes and subcutaneous tissue; skin closure with Nylon 4.0;
- External compressive bandage.
In the postoperative time, the external compressive bandage was maintained for 72 hours and the patient is requested to rest and avoid abdominal’s efforts/Valsalva. Figures 1a and b shows intraoperative images of case one, before and after meningocele correction. Both patients underwent this similar technique for correction of the meningocele, but few differences in mastoidectomy technique were made. Figures 2a and b shows computed tomography of ears and mastoid of case one pre surgery and post-surgery status. Long term fallow-up of 10 years showed no meningocele recurrence or middle ear effusion, and none of the patients presented new cases of meningitis.
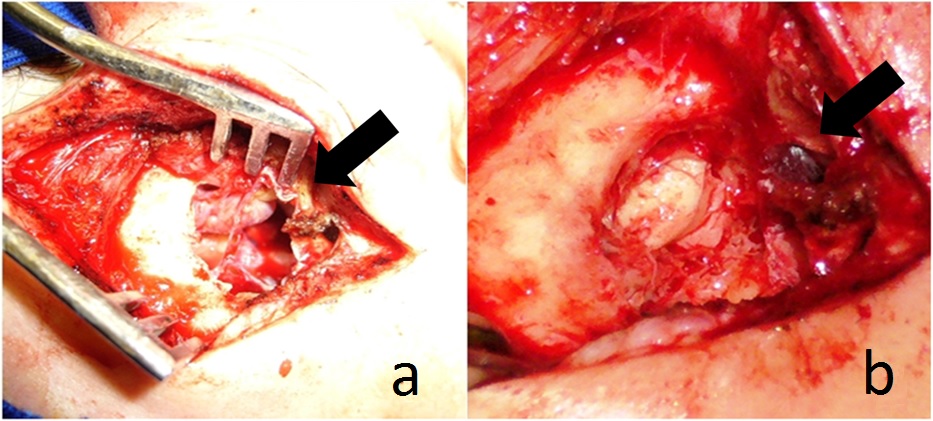
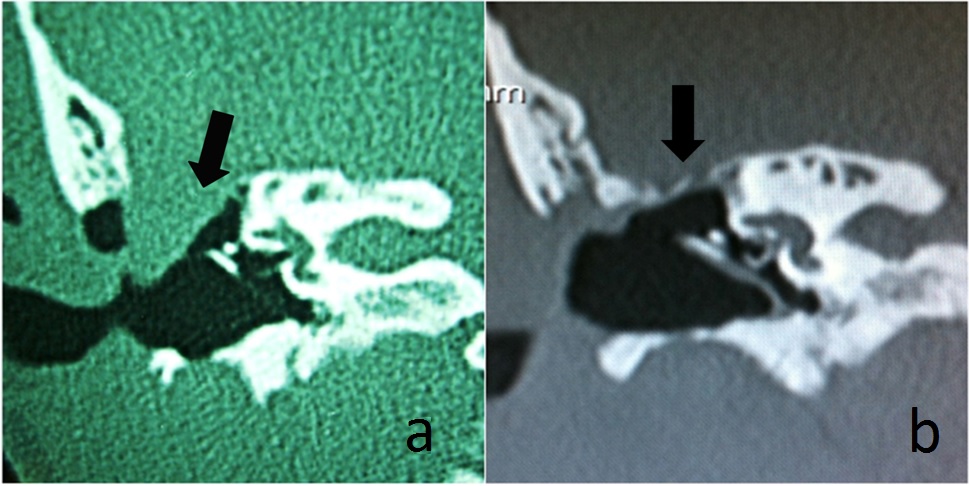
Figure 2: Computed tomography coronal plan of case one. Arrows point to pre-surgery status (3) and post-surgery status (4) of the tegmen with no residual meningocele.
DISCUSSION
Kasugai el al., [6] reported a case of meningocele who underwent repair surgery for the middle skull base defect with bone putty and covered by a pedunculated dermal flap of the temporal fascia after suturing the fistulous opening of duramater.
Kenning et al., [7] described a case series of 23 consecutive patients undergoing a combined mastoidectomy and middle cranial fossa craniotomy for the treatment of a tegmen defect. His technique involved a robust dural closure followed by extradural dissection and encephalocele reduction or resection. Both synthetic dural inlay and an epidural autologous graft along the tegmen were used to ensure that the areas of dural and osseous disruption are fully covered and reinforced [7].
Verma [8] described a case of meningocele that underwent mastoidectomy, followed by mass excision of the tumor, the bony defect was repaired in three tiers and superiorly wired mesh was placed covering the margins of the bony defect on all sides. This was followed by locally available conchal cartilage with intact mucoperichondrium on one side and then covered by a temporalis fascia graft tucked into the cranial and inferior side of the defect [8].
Mong et al., [9] described 2 cases of fallopian canal meningocele treated with combined transmastoid approach with middle fossa craniotomy, herniated tissue was amputated at the cranial base, and the defects were closed with condral cartilage, temporalis fascia, and middle turbinate mucosal-free grafts [9].
Savva et al., [10] published a series of 92 cases of temporal bone defects, in which 27 where traumatic cases and did not need surgery. The majority (79%) required a transmastoid approach alone. Similarly, all non-traumatic (spontaneous) CSF leaks required surgical closure involving mastoidectomy or a combined mastoid and middle fossa approach. Repairs were less likely to fail if supporting material was used, and better success rates were achieved when a multilayer technique was used to support the initial closure [10].
Nahas et al., [11] reported a series of 15 patients with spontaneous temporal meningocele all treated with combined transmastoid-middle fossa approach. It presented a success rate of 100%. Papanicolaou et al., [12] reported a case of meningocele treated with exploratory mastoidectomy, amputation of the herniated meningocele and closure of the defect with temporalis fascia and an inferiorly based pedunculated muscular flap [12].
Sergi et al., [13] reported 24 cases, all treated with transmastoid approach. In this study all cases had collagenous membrane used along with a bone graft, temporalis fascia and fibrin glue. No complications were demonstred in the medium 28 months follow-up [13].
We can notice from the literature that temporalis fascia along with condral cartilage are the most popular grafts, but mucosal flaps and other substances are often successful used to cover the bone defect.
We believe that there is much variability of the techniques presented, but there are some key points in common that may be responsible for the good successes presented by cited authors. A careful surgical dissection plus a definition of all meningocele, using some grafts and/or retails appears to be part of all the techniques presented.
In terms of surgical approach, the transmastoid technique has been shown safe and effective but finds its limitations according to the meningocele size. It seems that the most important factors considering success of the repair are multiple layers of supporting material as grafts, cartilage and others constituents.
Therefore, there are no significant differences between the kinds of repair material used, as long as the repair involves careful management and at least three kinds of different materials. Cartilage and fascia are a good example of effective and simple graft with great results in our patients and in the literature.
Finally, it is imperative to do a close follow-up to these patients controlling meningocele recurrence, hearing loss rehabilitation and risk factors control as cholesteatoma, weight gain, and trauma.
It is noteworthy that we found no description of techniques that had a surgical failure or need for rapprochement or further surgery.
CONCLUSION
COMPETING INTERESTS
REFERENCES
- Sanna M, Fois P, Russo A, Falcioni M (2009) Management of meningoencephalic herniation of the temporal bone: Personal experience and literature review. Laryngoscope 119: 1579-1585.
- Rao AK, Merenda DM, Wetmore SJ (2005) Diagnosis and management of spontaneous cerebrospinal fluid otorrhea. Otol Neurotol 26: 1171-1175.
- Kim L, Wisely CE, Dodson EE (2014) Transmastoid approach to spontaneous temporal bone cerebrospinal fluid leaks: hearing improvement and success of repair. Otolaryngol Head Neck Surg 150: 472-478.
- Alonso RC, de la Peña MJ, Caicoya AG, Rodriguez MR, Moreno EA, et al. (2013) Spontaneous skull base meningoencephaloceles and cerebrospinal fluid fistulas. Radiographics 33: 553-570.
- Kong WK, Lee CH, Eunhye Y, Shin SH (2014) Unruptured translabyrinthine meningocele without CSF otorrhea. Int J Pediatr Otorhinolaryngol 78: 566-569.
- Kasugai S, Kenmochi M, Nishino H, Okada T, Ohashi T (2003) A case of meningoencephalic herniation of the temporal bone. Auris Nasus Larynx 30: 103-105.
- Kenning TJ, Willcox TO, Artz GJ, Schiffmacher P, Farrell CJ, et al. (2012) Surgical management of temporal meningoencephaloceles, cerebrospinal fluid leaks, and intracranial hypertension: treatment paradigm and outcomes. Neurosurg Focus 32: 6.
- Verma R (2006) Meningoencephalocele of the middle ear cleft: Three tier management. Indian J Otolaryngol Head Neck Surg 58: 378-380.
- Mong S, Goldberg AN, Lustig LR (2009) Fallopian canal meningocele: report of two cases. Otol Neurotol 30: 525-528.
- Savva A, Taylor MJ, Beatty CW (2003) Management of cerebrospinal fluid leaks involving the temporal bone: report on 92 patients. Laryngoscope 113: 50-56.
- Nahas Z, Tatlipinar A, Limb CJ, Francis HW (2008) Spontaneous meningoencephalocele of the temporal bone: clinical spectrum and presentation. Arch Otolaryngol Head Neck Surg 134: 509-518.
- Papanikolaou V, Bibas A, Ferekidis E, Anagnostopoulou S, Xenellis J (2007) Idiopathic temporal bone encephalocele. Skull Base 17: 311-316.
- Sergi B, Passali GC, Picciotti PM, De Corso E, Paludetti G (2013) Transmastoid approach to repair meningoencephalic herniation in the middle ear. Acta Otorhinolaryngol Ital 33: 97-101.
Citation: Toro MDC, Guimarães AC, de Carvalho GM, Paschoal JR, Pfeilsticker LN (2016) Transmastoid Cartilage Graft-Meningocele Temporal: Surgical Approach. J Otolaryng Head Neck Surg 2: 005.
Copyright: © 2016 Mariana DC Toro, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.