Updating Information About the Burden of Meningococcal Disease Hospitalisations in Spain
*Corresponding Author(s):
Garrido-Estepa MNational Centre For Epidemiology, Preventive Medicine And Public Health, Carlos III Health Institute, Madrid, Spain
Tel:+34 918222974,
Fax:+34 913877816-15
Email:mgarrido@isciii.es; macarena.gaes@gmail.com
Abstract
Introduction
Meningococcal disease remains an important public health problem worldwide due to its high lethality and high sequelae rates. Although meningococcal disease shows a decreasing incidence trend, vaccination against the current predominant serogroup (serogroup B) in Europe is not offered by routine in Spain and continuous surveillance is needed.
Methods
Meningococcal disease (ICD-9: 036 codes in any diagnosis listed position) hospitalisations from 1997 to 2013 were obtained from the Spanish National Registry of Hospitalisations. Number of hospitalisations and deaths, hospitalisation and death rates, case fatality rates and average length of hospital stay were calculated for all meningococcal disease hospitalisations and for the main clinical presentations, meningitis and meningococcemia. Data on number of hospitalisations were compared to cases reported to the National Surveillance System.
Results
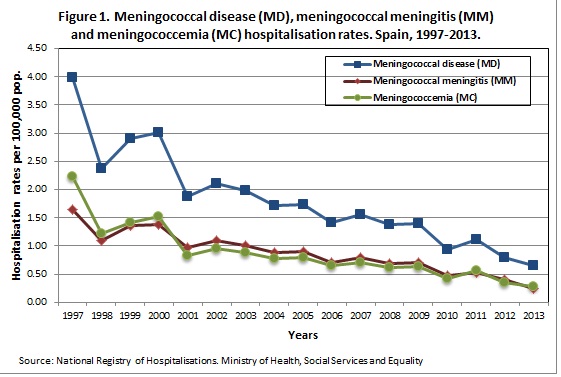
Between 1997 and 2013, there were 14,069 hospital discharges due to meningococcal disease. Of them, 13,267 (94.30%) were first hospitalisations and 802 (5.70%) readmissions/transfers. Most common clinical presentation were meningococcemia alone (41.04%; 5,774 hospitalisations), followed by meningitis alone (39.61%; 5,573 hospitalisations). Both clinical presentations appeared together in 1,885 (13.40%) hospitalisations. Hospitalisation rates decreased (p<0.001) from 1997 to 2013 from 3.98 to 0.65; from 1.65 to 0.25; and from 2.23 to 0.27 hospitalisations per 100,000 population for meningococcal disease, meningitis and meningococcemia, respectively. Case fatality rate was 7.31% for all, 3.88% for meningitis and 9.56% for meningococcemia. Meningococcemia showed higher hospitalisation and death rates in 1-4 and 5-14 age-groups (p<0.001) and higher case fatality rate in all age-groups (p<0.001) than meningitis. Average length of stay was 11.46 days. High concordance (98%) among the National Surveillance System and the National Registry of Hospitalisation was found. Serogroup B cases notified decreased from 458 in 1997 to 193 cases in 2013.
Discussion
Meningococcemia is the most frequent clinical presentation in Spain with higher hospitalisation and death rates in the youngest groups and higher case fatality rates than the other predominant clinical presentation, meningitis. Meningococcal disease shows a decreasing trend and serogroup B cases decreased by 58% from 1997 to 2013 in absence of vaccination.
INTRODUCTION
Neisseria meningitidis is an important cause of meningitis and septicaemia, with complications including deafness, disability or death [1]. Despite the success in reducing Invasive Meningococcal Disease (IMD) incidence and in developing vaccines against meningococcal serogroups A, C, W and Y [2], the development of a vaccine against meningococcus B has been a challenge [3,4]. In 2013 a new serogroup B vaccine has been approved for use in Europe, but only United Kingdom has recommended its introduction into the routine infant schedule [5], in Spain it was introduced with hospital use only until the 1st of October, 2015 in which prescription was authorized but not funded [6]. Serogroup B is the predominant serogroup causing meningococcal disease at the moment in Europe. Nevertheless, serogroup B shows a decreasing trend in incidence parallel to serogroup C in most of the European countries [7] that it is attributed to a secular trend [8].
Similar situation was observed in Spain. Introduction of serogroup C conjugate vaccine in 2000 in the routine infant schedule and the development of different catch-up campaigns has resulted in an important decrease in incidence by this serogroup, with most of the remaining cases in older ages not targeted by any vaccination program [9]. Serogroup B incidence has decreased also, but it still accounted the 71% of the cases notified in 2012-2013 season to the Spanish National Surveillance System [10].
Nevertheless, other countries, as Canada, did not experience the same situation. A recent report from the Public Health Agency of Canada showed a decreasing trend of serogroup C after the introduction of serogroup C vaccination in the routine childhood immunization programs in 2007, however, serogroup B did not change across the 2006 and 2011 period [11].
Current information of the disease is necessary for the reassessment of the preventive measures. Hospitalisation burden of the disease was reviewed previously by Gil-Prieto et al. [12] including 1997-2008 period. The aim of this study is to update the information on hospitalisations associated to meningococcal disease. For that, we carried out a retrospective study of the hospitalisations for meningococcal disease in Spain between 1997 and 2013. Length of hospital stay, number of hospitalisations and death rates, as well as Case Fatality Rates (CFR), are useful parameters to evaluate the need and the cost-effectiveness of the preventive measures.
METHODS
All hospital discharges with 036 (meningococcal disease) ICD-9 codes in any diagnosis listed position were included in our study between 1997 and 2013:
- 036.0: Meningococcal meningitis
- 036.1: Meningococcal encephalitis
- 036.2: Meningococcemia
- 036.3: Waterhouse-Friderichsen syndrome
- 036.4: Meningococcal carditis, unspecified, meningococcal pericarditis, meningococcal endocarditis, meningococcal myocarditis
- 036.8: Other meningococcal infections (optic neuritis and meningococcal arthropathy)
- 036.9: Meningococcal infection, unspecified
Statistical methods
Number of hospitalisations and hospitalisation rates (per 100,000 population) for meningococcal disease were calculated by year, clinical presentation and age group. Additionally, deaths, mortality rates (per 100,000 population), CFR and average length of hospital stay were calculated by age-groups and clinical presentation.
The National Registry of Hospitalisations is a discharge database and the date used in this article is the date of discharge in order to evaluate the burden of the disease at hospital level. However, when we compared data from the National Registry of Hospitalisations with data from the National Surveillance System (incidence database) we used date (year) of hospitalisation instead of date of discharge to allow the comparisons with date of symptoms onset provided by the National Surveillance System.
Population used to calculate rates was obtained from the National Institute of Statistics.
Differences in proportions were assessed by the Chi-square test and the exact test of Fisher, if necessary. Differences in means were assessed by using the t test. To compare the changes in hospitalisation rates over time, we created two periods, pre-vaccination (1998-2000) and the latest period (2010-2013). We excluded year 1997 from the pre-vaccination period because there was an increased incidence due to a hyper-virulent strain of serogroup C that could help to overestimate the decrease of the disease [13,14]. Hospitalisation Rate Ratios (HRR) and their Confidence Intervals at 95% (CI95%) comparing the latest period with the pre-vaccination period (Reference) were calculated using Poisson regression. Statistical significance was considered when p-value was <0.05. All analyses were performed using Stata v. 13 and Excel v. 7.0.
RESULTS
Therefore, 14,069 hospitalisations discharges were included. Of them, 13,267 (94.30%) were first admissions and 802 (5.70%) were classified as readmissions or hospital transfers. In 13,032 (92.63%) hospitalisations the main diagnose was meningococcal disease infection (036 codes) while in 1,037 (7.37%) meningococcal disease codes were included as secondary diagnoses.
Mean age (Standard Deviation: SD) of patients (excluding readmissions) was 17.83 (SD: 23.18) and median age was 6.25 (Interquartile range: 1.62-23.20) years old. Distribution of hospitalisations was similar by sex: 50.78% (6,737) were males, 49.18% (6,524) females and 0.03% (4) had missing information. Sex ratio (male/female) by age-group decreases with age (p<0.001): from 1.24 in the 64 years age-group. Men proportion was statistically higher in the 64 age groups, with similar distribution of men vs. women in the rest of the groups. The average length of stay was 11.46 days (SD: 12.95). Death outcome was register in 1,028 patients (7.75%; 1,028/13,267 patients).
Table 1 shows the distribution of hospitalisations in any diagnosis listed position due to MD infection by clinical presentation during the study period. From all hospitalisations, 2,085/14,069 (14.82%) presented more than one clinical presentation. Meningococcal Meningitis (MM) and Meningococcemia (MC) clinical presentations appeared together in 1,885/14,069 (13.40%) hospitalisations. Only in 884/14,069 (6.28%) hospitalisations MM or MC did not appear as clinical presentation.
| ICD-9: 036 | N | Percentage (%) |
| Meningococcal meningitis (036.0) | 7458 | 53.01 |
| Meningococcal encephalitis (036.1) | 169 | 1.20 |
| Meningococcemia (036.2) | 7659 | 54.44 |
| Waterhouse-Friderichsen syndrome (036.3) | 133 | 0.95 |
| Meningococcal carditis (036.4) | 39 | 0.28 |
| Other meningococcal infections (036.8) | 346 | 2.46 |
| -Neuritis (036.81) | 7 | 0.05 |
| -Arthropathy (036.82) | 104 | 0.74 |
| -Others (036.89) | 235 | 1.67 |
| Meningococcal infection, unspecified (036.9) | 395 | 2.81 |
| *Total number of hospitalizations (N=14,069) are not the sum of clinical presentations. Some patient presented more than one clinical presentation | ||
Meningococcal disease hospitalisation rates
Hospitalisation rates by age-groups
| Age-groups | MD | MM | MC | |||
| N | Rates (CI95%) | N | Rates (CI95%) | N | Rates (CI95%) | |
| 248633.24 (31.94; 34.57)131817.62 (16.68; 18.60)139118.60 (17.63; 19.60) | ||||||
| 1-4 y. | 4127 | 14.04 (13.62; 14.48) | 1880 | 6.40 (6.11; 6.69) | 2734 | 9.30 (8.96; 9.66) |
| 5-14 y. | 2497 | 3.45 (3.31; 3.59) | 1196 | 1.65 (1.56; 1.75) | 1591 | 2.20 (2.09; 2.31) |
| 15-24 y. | 1755 | 1.94 (1.85; 2.03) | 1201 | 1.33 (1.25; 1.41) | 703 | 0.78 (0.72; 0.84) |
| 25-44 y. | 1076 | 0.45 (0.43; 0.48) | 692 | 0.29 (0.27; 0.31) | 398 | 0.17 (0.15; 0.19) |
| 45-64 y. | 1037 | 0.59 (0.56; 0.63) | 603 | 0.35 (0.32; 0.37) | 411 | 0.24 (0.21; 0.26) |
| >64 y. | 1085 | 0.88 (0.82; 0.93) | 563 | 0.45 (0.42; 0.49) | 430 | 0.35 (0.31; 0.38) |
| Total | 14069 | 1.91 (1.88; 1.95) | 7453 | 1.01 (0.99; 1.04) | 7658 | 1.04 (1.02; 1.07) |
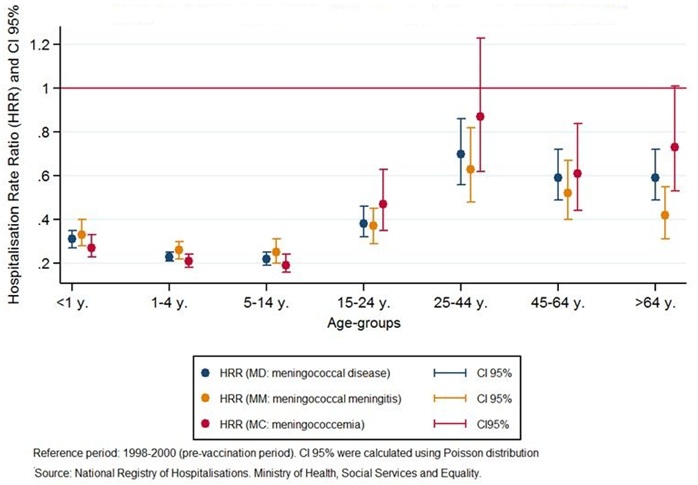 Figure 2: Hospitalisation Rate Ratios (HRR, CI95%) for Meningococcal Disease (MD), Meningococcal Meningitis (MM) and Meningococcemia (MC) in any diagnosis listed position comparing the last period (2010-2013) with the pre-vaccination period (1998-2000).
Figure 2: Hospitalisation Rate Ratios (HRR, CI95%) for Meningococcal Disease (MD), Meningococcal Meningitis (MM) and Meningococcemia (MC) in any diagnosis listed position comparing the last period (2010-2013) with the pre-vaccination period (1998-2000).Mortality rates and Case Fatality Rates (CFR)
| Deaths | Mortality Rate (per 100.000 pop) (CI 95%) |
Case fatality Rate % (CFR) (CI 95%) |
|||||||
| Age groups | MD | MM | MC | MD | MM | MC | MD | MM | MC |
| 12320971.64 (1.37; 1.96)0.27 (0.16; 0.41)1.30 (1.05; 1.58)4.95 (4.11; 5.90)1.52 (0.93; 2.34)6.97 (5.65; 8.51) | |||||||||
| 1-4 y. | 199 | 25 | 178 | 0.68 (0.59; 0.78) | 0.09 (0.06; 0.13) | 0.61 (0.52; 0.70) | 4.82 (4.18; 5.54) | 1.33 (0.86; 1.96) | 6.51 (5.59; 7.54) |
| 5-14 y. | 100 | 29 | 77 | 0.14 (0.11: 0.17) | 0.04 (0.03; 0.06) | 0.11 (0.08; 0.13) | 4.00 (3.26; 4.87) | 2.42 (1.62; 3.48) | 4.84 (3.82; 6.05) |
| 15-24 y. | 160 | 54 | 110 | 0.18 (0.15; 0.20) | 0.06 (0.04; 0.08) | 0.12 (0.10; 0.15) | 9.12 (7.76; 10.64) | 4.50 (3.38; 5.87) | 15.65 (12.86; 18.86) |
| 25-44 y. | 105 | 31 | 70 | 0.04 (0.04; 0.05) | 0.013 (0.089; 0.019) | 0.03 (0.02; 0.04) | 9.76 (7.98; 11.81) | 4.48 (3.04; 6.36) | 17.59 (13.71; 22.22) |
| 45-64 y. | 131 | 41 | 91 | 0.07 (0.06; 0.09) | 0.023 (0.017; 0.032) | 0.052 (0.042; 0.064) | 12.63 (10.56; 14.99) | 6.80 (4.88; 9.22) | 22.14 (17.83; 27.18) |
| >64 y. | 210 | 89 | 109 | 0.17 (0.15; 0.19) | 0.07 (0.06; 0.09) | 0.09 (0.07; 0.11) | 19.35 (16.83; 22.16) | 15.81 (12.70; 19.45) | 25.35 (20.81; 30.58) |
| Total | 1028 | 289 | 732 | 0.14 (0.13; 0.15) |
0.039 (0.035; 0.044) |
0.10 (0.09; 0.11) | 7.31 (6.87; 7.77) | 3.88 (3.44; 4.35) | 9.56 (8.88; 10.28) |
Length of stay
| Age-group | MD (SD) | MM (SD) | MC (SD) |
| 10.52 (9.57)11.44 (9.33)10.15 (9.94) | |||
| 1-4 y. | 9.50 (10.42) | 9.11 (6.67) | 9.84 (11.92) |
| 5-14 y. | 9.60 (9.21) | 9.28 (7.02) | 9.90 (9.92) |
| 15-24 y. | 12.02 (12.30) | 11.29 (8.00) | 13.23 (16.03) |
| 25-44 y. | 14.88 (19.78) | 14.27 (13.31) | 16.17 (23.41) |
| 45-64 y. | 17.03 (20.44) | 16.40 (17.05) | 17.96 (24.38) |
| >64 y. | 15.76 (15.55) | 17.13 (15.34) | 14.40 (16.14) |
| Total | 11.46 (12.95) | 11.58 (10.47) | 11.24 (13.91) |
Comparison among the National Surveillance System and the National Registry of Hospitalisations
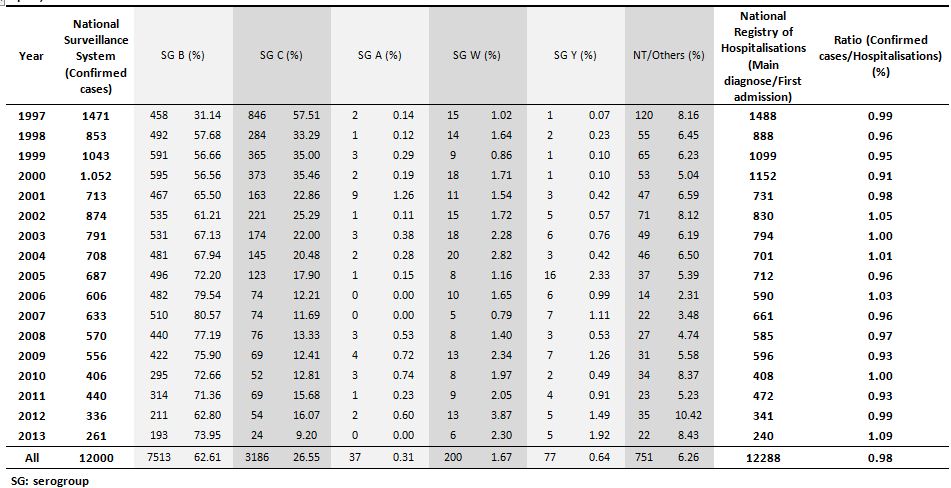 Table 5: Number of confirmed cases (overall and by serogroup) notified to the National Surveillance System, number of hospitalisations related to Meningococcal Disease (MD) as main diagnose and first admission registered in the National Registry of Hospitalisations and the ratio between confirmed cases and hospitalisations. Spain, 1997-2013.
Table 5: Number of confirmed cases (overall and by serogroup) notified to the National Surveillance System, number of hospitalisations related to Meningococcal Disease (MD) as main diagnose and first admission registered in the National Registry of Hospitalisations and the ratio between confirmed cases and hospitalisations. Spain, 1997-2013.In 1997 serogroup C was more frequent than serogroup B (57.51% vs. 31.14%). However, after 1997 that was still influenced by the presence of a hyper-virulent strain of serogroup C, serogroup C proportion decreased up to 9.20% in 2013. For the whole study period, serogroup B was the predominant serogroup (62.61% of the cases), followed by serogroup C (26.55%). Serogroup A (0.31), serogroup W (1.67%) and serogroup Y (0.64%) were rare.
DISCUSSION
This study describes the burden of hospitalisations related to meningococcal disease and the changes occurred in the disease due to the different public health control and preventive measures. It actualizes also the previous study developed by Gil-Prieto et al., [12] that covered 1997-2008 period. Although, Gil-Prieto et al., included the first years of this study it is important to take into account that we carried out a previous data cleaning to identify possible duplicates and readmission/hospital transfers. This is important because due to the severity of meningococcal disease and, sometimes, the long periods for recovering, we expected hospital transfers to different units or hospitals and readmissions to continue sequelae treatments. Moreover, readmissions/hospital transfers identification was essential to allow comparisons between the hospitalisations and the cases notified (incidence) of the disease. After data cleaning, we detected only 0.23% of duplicates (most of them concentrated in the first years) showing the high reliability of the registry. Additionally, we identified 5.70% readmissions/hospital transfers.
Regarding to meningococcal disease hospitalisations, we observed an irregular decreasing trend in the hospitalisation rates since 1997. That decrease was more accentuated after 2000, mostly due to the implementation of the conjugated vaccine for meningococcal C serogroup in the National Vaccination Programs. The decrease in meningococcal disease has been described in most European countries [7] and although it has been more marked in the serogroup C due to vaccination programs, it has been also reported in serogroup B. Independently, of the reduction in serogroup B incidence, this serogroup is still the main cause of meningococcal disease, up to 71% of the cases in Spain in 2012-2013 season [10]. In Spain vaccination against serogroup B has been approved only for hospital use [15,16] until the 1st of October of 2015 in which prescription was approved (but not funded) [6]. A study, carried out with samples from different European countries gave estimated strain coverage of 69% (CI95% 48-85) for Spanish isolates [17] and cost-effectiveness of the vaccine has been controversial due to high cost of the vaccine and low incidence [18-20].
We found that sex ratio of hospitalisation was over 1 (p<0.001) in <1 and 1-4 years age-groups and decreases with age. In older groups were women who were mostly affected (Sex ratio>64 years= 0.47). However those results are related with higher number of men births and higher women survival, so therefore should be taken cautiously.
From all hospitalisations, 93.72% were due to MM and/or MC and only 6.28% hospitalisations were related to other clinical presentations. Higher meningeal tropism has been reported in other studies resulting in higher proportion of MM compared to MC [21], however in Spain we have higher proportion of MC. That is important if we considered differences in outcomes. MM and MC showed a similar decreasing trends, and both presented the highest hospitalisation and mortality rates in <1 year age-group, but we found that MC showed higher hospitalisation rates in 1-4 and 5-14 age-groups than MM. Additionally, MC due to its seriousness also presented higher mortality rates and CFR than MM, not exclusively in the youngest age-groups (<1, 1-4 and 5-14 years age-groups), but in all age-groups.
In spite of improvement in diagnose and treatments, overall CFR has remained around 7-8% in Europe in the last years [22], similarly to our results in which overall CFR was 7.31%. Although mortality rates are higher at younger ages because hospitalisation rate is also high in infants, CFR increased with age for all, MM and MC. Similarly, length of stay increased with age, although it was higher in <1 year than in 1-4 and 5-14 years age-group.
Hospital discharges with meningococcal codes as secondary diagnoses were associated with shock, unspecified agents or other specified agents (including HIV). Due to the severity of the disease we expected main diagnoses related to acute symptoms while meningococcal disease is confirmed. Additionally, relationship of meningococcal disease with concomitant infections [23-25] and immunodeficiency [26,27] has been described previously.
When we compared confirmed cases reported to the National Surveillance System and hospitalisations (first admission and main diagnoses) included in the National Registry of Hospitalisations overall ratio found was 0.98. That implies a very good coherence in between both, the National Surveillance System and the National Registry of Hospitalisations. We have to consider that the National Registry of Hospitalisations is a discharge database and year 2013 admissions could be slightly higher when 2014 database will be available. Although, the National Registry of Hospitalisations does not provide information of serogroup, in the hospital practice Neisseria meningitidis infection is confirmed through blood culture or lumbar punction and samples are sent to the Reference Laboratories to more specific strain determination. Therefore we expected good coherence among both databases.
Some limitations derived from the use of the National Registry of Hospitalisations were presented in previous studies [12,28]. However, introduction of new technologies and computerization in data management has improved notably the quality of this registry in the last years. Additionally, one of the strength of our study is the evaluation of the quality of the data previous to our analyses which showed a low number of duplicates and a high concordance with the National Surveillance System when transfers/readmissions were identified. Valuable information can be obtained combining epidemiological information with information collected during the hospitalisation to improve the knowledge of the disease.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
The authors declare no conflicts of interest.
- Rosenstein NE, Perkins BA, Stephens DS, Popovic T, Hughes JM (2001) Meningococcal disease. N Engl J Med 344: 1378-1388.
- Halperin SA, Bettinger JA, Greenwood B, Harrison LH, Jelfs J, et al. (2012) The changing and dynamic epidemiology of meningococcal disease. Vaccine 30: 26-36.
- Sadarangani M, Pollard AJ (2010) Serogroup B meningococcal vaccines-an unfinished story. Lancet Infect Dis 10: 112-124.
- Tan LK, Carlone GM, Borrow R (2010) Advances in the development of vaccines against Neisseria meningitidis. N Engl J Med 362: 1511-1520.
- Pollard AJ, Riordan A, Ramsay M (2014) Group B meningococcal vaccine: recommendations for UK use. Lancet 383: 1103-1104.
- Press note: Pharmacies are authorized to sell vaccine against meningitis B from October 1st. Ministry of Health, Social Services and Equality, Madrid, Spain.
- European Centre for Disease Prevention and Control (2014) Annual epidemiological report -vaccine-preventable diseases - invasive bacterial diseases. European Centre for Disease Prevention and Control, Sweden.
- Alonso JM, Gilmet G, Rouzic EM, Nassif X, Plotkin SA, et al. (2007) Workshop on vaccine pressure and Neisseria meningitidis, Annecy, France, 9-11 March 2005. Vaccine 25: 4125-4129.
- Garrido-Estepa M, León-Gómez I, Herruzo R, Cano R (2014) Changes in meningococcal C epidemiology and vaccine effectiveness after vaccine introduction and schedule modification. Vaccine 32: 2604-2609.
- Garrido-Estepa M, Maguiña Gúzman M, Cano R (2014) Enfermedad meningocócica en España. Análisis de la temporada 2012-2013. Centro Nacional de Epidemiología, España.
- Li YA, Tsang R, Desai S, Dehaan H (2014) Enhanced surveillance of invasive meningococcal disease in Canada, 2006-2011. Canada Communicable Disease Report CCDR 40-49.
- Gil-Prieto R, García-García L, Alvaro-Meca A, González-Escalada A, Viguera Ester P, et al. (2011) The burden of hospitalizations for meningococcal infection in Spain (1997-2008). Vaccine 29: 5765-5770.
- Berrón S, De La Fuente L, Martín E, Vázquez JA (1998) Increasing incidence of meningococcal disease in Spain associated with a new variant of serogroup C. Eur J Clin Microbiol Infect Dis 17: 85-89.
- Mateo S, Cano R, Garcia C (1997) Changing epidemiology of meningococcal disease in Spain, 1989-1997. Euro Surveill 2: 71-74.
- Grupo de trabajo MenB (2013) Vacuna frente a enfermedad meningocócica invasora por serogrupo B y su posible utilización en Salud Pública. Comisión de Salud Pública del Consejo Interterritorial del Sistema Nacional de Salud, Ministerio de Sanidad, Servicios Sociales e Igualdad.
- Sánchez AL, Navarro-Alonso JA, Salmerón García F (2014) Immunisation against meningococcus B: the case of Spain. Lancet 383: 217-218.
- Vogel U, Taha MK, Vazquez JA, Findlow J, Claus H, et al. (2013) Predicted strain coverage of a meningococcal multicomponent vaccine (4CMenB) in Europe: a qualitative and quantitative assessment. Lancet Infect Dis 13: 416-425.
- Christensen H, Hickman M, Edmunds WJ, Trotter CL (2013) Introducing vaccination against serogroup B meningococcal disease: an economic and mathematical modelling study of potential impact. Vaccine 31: 2638-2646.
- Christensen H, Trotter CL, Hickman M, Edmunds WJ (2014) Re-evaluating cost effectiveness of universal meningitis vaccination (Bexsero) in England: modelling study. BMJ 349: 5725.
- Tu HA, Deeks SL, Morris SK, Strifler L, Crowcroft N, et al. (2014) Economic evaluation of meningococcal serogroup B childhood vaccination in Ontario, Canada. Vaccine 32: 5436-5446.
- Pace D, Pollard AJ (2012) Meningococcal disease: clinical presentation and sequelae. Vaccine 30: 3-9.
- European Centre for Disease Prevention and Control (2012) Annual epidemiological report. Reporting on 2010 surveillance data and 2011 epidemic intelligence data. European Centre for Disease Prevention and Control, Sweden.
- Jacobs JH, Viboud C, Tchetgen ET, Schwartz J, Steiner C, et al. (2014) The association of meningococcal disease with influenza in the United States, 1989-2009. PLoS One 9: 107486.
- Loh E, Kugelberg E, Tracy A, Zhang Q, Gollan B, et al. (2013) Temperature triggers immune evasion by Neisseria meningitidis. Nature 502: 237-240.
- Tuite AR, Kinlin LM, Kuster SP, Jamieson F, Kwong JC, et al. (2010) Respiratory virus infection and risk of invasive meningococcal disease in central Ontario, Canada. PLoS One 5: 15493.
- Foster RA, Carlring J, Lees A, Borrow R, Ramsay M, et al. (2010) Functional T-cell deficiency in adolescents who experience serogroup C meningococcal disease despite receiving the meningococcal serogroup C conjugate vaccine. Clin Vaccine Immunol 17: 1104-1110.
- Rezaei N, Siadat SD, Aghamohammadi A, Moin M, Pourpak Z, et al. (2010) Serum bactericidal antibody response 1 year after meningococcal polysaccharide vaccination of patients with common variable immunodeficiency. Clin Vaccine Immunol 17: 524-528.
- Peiró S, Librero J (1999) [The quality assessment from the minimum basic hospital discharge data set]. Rev Neurol 29: 651-661.
Citation: Ordóñez-León GY, Martínez EV, Herruzo R, Garrido-Estepa M (2016) Updating Information About the Burden of Meningococcal Disease Hospitalisations in Spain. J Vaccines Res Vaccin 2: 003.
Copyright: © 2016 Ordóñez-León GY, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.