
Evidence-based practical Guideline on the Management of Failed Spinal Anesthesia in pregnant mothers undergoing Caesarean Section in a Resource constrained area; Systematic Review Article
*Corresponding Author(s):
Tajera Tageza IlalaDepartment Of Anesthesia, College Of Medicine And Health Science, Hawassa University, Hawassa, Ethiopia
Email:tajeratageza@gmail.com
Abstract
Background
Neuroaxial anesthesia is regarded as the most effective form of anesthesia for cesarean procedures. Although generally reliable, Neuraxial operations can fail totally or partially and may need further assistance. After caesarean sections under neuroaxial anesthesia, pain has replaced unintended awareness under general anesthesia as the most common successful medicolegal claim against obstetric anesthetists. The objective of this guideline is to support medical professionals and promote practice uniformity in this area by evaluating the causes, types, and treatments of spinal anesthesia failure.
Methodology
We searched PubMed, Cochran Library, and Google Scholar for articles that have been published up to 2022. Spinal anesthesia AND cesarean section OR failed spinal anesthesia OR inadequate spinal anesthesia OR neuroaxial anesthesia and pain management OR anesthesia technique OR anesthesia management OR analgesia technique were the search terms used in PubMed and Cochrane, and full sentences were searched in Google Scholar. On the basis of the included studies, recommendations were generated for the 21 publications that resulted after they had been evaluated for relevance. This review covered entire articles published up to 2022 that were written in the English language, observational, interventional, meta-analysis, and systematic review research.
Conclusion
We recommend appropriate communication between the anesthetist and woman in addition to the practical aspects of block assessment. A good communication between the woman and anesthetist may improve the accuracy of sensory assessment. Appropriate assessment and testing of a neuroaxial block is very important to make the right decision. It is also essential that the assessment of the neuroaxial block is comprehensively and accurately documented. Acknowledge any complaint of pain or distress and ask the surgeon to stop if safe, then use intravenous fast-acting opioids or ketamine in the first instance. A request for general anesthesia should be honoured if possible. It is good practice for the anesthetist to recommend general anesthesia if effective analgesia is unlikely to be achieved using other methods. Any patient who feels pain during caesarean section should be followed-up before they leave hospital by a senior anesthetist, who should also contact the patient's general practitioner.
Keywords
Cerebrospinalfluid; Combined Spinal-Epidural; Neuroaxial anesthesia
Abbreviations
CSE: Combined Spinal-Epidural
GA: General Anesthesia
GOE: Grade of Evidence
LOE: Level of Evidence
RCT: Randomized Control Trial
Introduction
Spinal anesthesia is a neuroaxial anesthesia technique in which local anesthetic is placed directly the intrathecal space (subarachnoid space). The subarachnoid space houses sterile cerebrospinal fluid (CSF), the clear fluid that bathes the brain and spinal cord [1]. Regional anesthesia for a caesarean section provides a rapid, predictable and reliable block for surgery, as well as providing excellent post-operative analgesia. It allows the mother to remain awake during the delivery and thus provides the emotional and psychological benefits of this [2].
Failure of spinal anesthesia may be partial or complete. Complete failure is defined as the absence of sensory or motor blockade, and partial failure is defined as insufficient level, quality, or duration of drug action for that particular surgery [3,4]. Failure of regional anesthesia for a caesarean section can be described in a number of ways. The commonest definitions include failure to provide adequate surgical conditions and/or maternal discomfort or pain during a caesarean section, with or without the need to convert to a GA [4,5]. While in some situations converting to a general anesthetic is prudent, poor block assessment or suboptimal attempts to correct an inadequate block can lead to unnecessary abandonment of regional anesthesia. Assessment of the block following neuroaxial anesthesia is essential to minimize the risk of an inadequate block, but objective assessment can be challenging [5,6].
Motor block in association with epidural or spinal anesthesia is frequently described in terms of the Bromage score. To assess the sensory block there are four possible end points
- total loss of all sensation to the pin;
- the pin is recognized as a touch sensation but is not ecognized as being sharp
- the pin is recognized as being sharp but is less sharp than normal; or the pinprick feels normal [7].
Inadequate neuroaxial anesthesia, defined as the need to convert to general an aesthesia; the need to repeat or abandon a planned primary neuroaxial technique following incision; unplanned administration of intra-operative analgesia (excluding sedatives); or unplanned epidural drug supplementation [6,8].
Justification
The best type of anesthesia for cesarean sections is recognized as neuroaxial anesthesia. Neuroaxial procedures can fail completely or partially, while being typically trustworthy, and additional support may be required. Thus, pain supplanted unintentional awareness under general anesthesia as the most frequent successful medicolegal claim against obstetric anesthetists after caesarean sections under neuroaxial anesthesia.
A woman is at risk of having negative psychological effects if she feels pain during a caesarean section while under neuroaxial anesthesia. As the most frequent and successful medical-legal claim against obstetric anesthetists, litigation deriving from pain after caesarean section under neuroaxial anesthesia has supplanted inadvertent awareness under general anesthesia. Numerous factors were taken into account, including blood found in the cerebrospinal fluid, an emergency cesarean section, numerous trials, the dosage of bupivacaine, the length of the procedure, any previous anesthesia, the type and size of the spinal needle, and the basicity of bupivacaine. Due to the intense pressure of failing spinal anesthetic, this has happened. Therefore, it is essential to properly measure and control pain after a cesarean section under spinal anesthesia. The present guideline also incorporates the needs of smooth communication between the anesthetist and woman in addition to our clinical decision and also the postoperative follow-up of women with intraoperative pain.
The objective this guideline is to evaluate the types and management of spinal anesthesia failure and the co-factors of spinal anesthesia failure and support doctors and encourage practice uniformity in this field by evaluating the causes, types, and therapy of spinal anesthetic failure.
Methodology
We performed a literature search in GOOGLE SCHOLAR, Cochran library and PubMed for material published up to 2022.The search performed using key words for PubMed and Cochrane [spinal anesthesia AND cesarean section OR failed spinal anesthesia or inadequate spinal anesthesia or neuroaxial anesthesia and pain management OR anesthesia technique OR anesthesia management OR analgesia technique] and by using full sentences search for google scholar. The resulting publications were assessed for relevance and Recommendations were developed on the basis of the included researches as described as shown in (Table 1)
|
Level of evidence |
Grading criteria |
Grade of recommendation |
|
1a |
Systematic reviews of RCTs including meta-analysis |
A |
|
1b |
Individual RCT with narrow confidence interval |
A |
|
1c |
All or none randomized controlled trials |
B |
|
2a 2b
|
Systematic review of cohort study Individual cohort including low quality RCT |
B |
|
2c |
Outcome research study |
C |
|
3a |
Systematic review of case control studies |
C |
|
3b |
Individual case control study |
C |
|
4 |
Case series, poor quality cohort and case control studies |
C |
|
5 |
Expert opinion without explicit critical appraisal, or based on physiology, bench research or “first principles” |
D |
Table 1: Levels of Evidences and Grades of Recommendations Discussion.
Observational, cohort studies, interventional studies, meta-analysis and systematic review studies, full articles published up to 2022 and articles written in English language were included in this review as shown by (Figure 1 & Table 2)
|
SNo |
Author/ Year |
Study |
Design |
Findings of the studies |
|
1
|
Jones GWet al,2017 |
Management of failed spinal anesthesia for caesarean section. |
Cross-sectional |
There is a need for standardized assessment of the adequacy of spinal anesthesia for CS in SA, as well as a failed spinal algorithm. |
|
2 |
Rukewe A,et al,2015 |
Failed obstetric spinal anesthesia in a Nigerian teaching hospital: incidence and risk factors. |
|
both pharmacological and non-pharmacological treatment methods are effective in relieving and reducing a range of pediatric pain diseases, |
|
3 |
Fettes PDW, etal, 2009 |
Failed spinal anesthesia: mechanisms, management, and prevention. |
Systematic review |
Options for managing an inadequate block include repeating the injection, manipulation of the patient's posture to encourage wider spread of the injected solution, supplementation with local anesthetic infiltration by the surgeon, use of systemic sedation or analgesic drugs, and recourse to general anesthesia. |
|
4 |
Husain T,et al,2010 |
How UK obstetric anesthetists assess neuroaxial anesthesia for caesarean delivery: |
Survey |
Compared to all other methods of assessing neuroaxial block, ethyl chloride was the most popular in 2004 |
|
5 |
Bourne TM, et al,1997 |
A survey of how British obstetric anesthetists test regional anesthesia before caesarean section |
Survey |
Temperature sensation was the most common sensory modality tested (64%) and 79% of those who tested for temperature sensation used an ethyl chloride spray. |
|
6 |
Hoyle J,et al,2015 |
Assessing the height of block for caesarean section over the past three decades: trends from the literature |
Systematic review |
the method of assessing motor block, with most of those that did describing it as the 'Bromage scale', |
|
7 |
Nor NM. et al,2013 |
Assessing blocks after spinal anesthesia for elective caesarean section: |
30, RCT |
Block level assessment methods using first sharp and touch same as control were equivalent |
|
8 |
Kocarev M, et al,2010 |
Sensory testing of spinal anesthesia for caesarean section: differential block and variability |
RCT |
Tests for light touch showed the least variability. More expensive tests do not appear to have any advantage over the least expensive test, cotton wool. |
|
9 |
Russell IF,2004 |
A comparison of cold, pinprick and touch for assessing the level of spinal block at caesarean section. |
Comparative study |
The results suggest that, for clinical purposes, there is no difference in outcomes whether Neurotip touch or ethyl chloride spray touch sensations are used |
|
10 |
Ousley Ret al, 2012 |
Assessment of block height for satisfactory spinal anesthesia for caesarean section. |
Observational study |
All women had satisfactory anesthesia despite having a block to touch below T6. Single modality assessment of block height, particularly using touch, may erroneously indicate inadequate anesthesia for caesarean section. |
|
11 |
Russell IF, 1995 |
Levels of anesthesia and intraoperative pain at caesarean section under regional block. |
Cross-sectional |
Assessing the adequacy of block by sharp pin prick may be misleading and that in the absence of spinal or epidural narcotics a level of anesthesia up to and including T5 is required to prevent pain during caesarean section. |
|
12 |
Brull SJ.et al, 1989 |
Time-courses of zones of differential sensory blockade during spinal anesthesia with hyper baric tetracaine or bupivacaine |
Comparative study |
zones of differential sensory blockade are essentially the same with tetracaine and bupivacaine |
|
13 |
A.A. Abraham,et al,2013 |
Failed spinal anesthesia- management by giving a second spinal |
Prospective cohort |
Repeating a spinal anesthesia after a failed one is a good method of management, if conditions permit. |
|
14 |
M. Simeen, et al,2017 |
An observational prospective cohort study of incidence of spinal failure and Need of Supplement, |
prospective cohort study |
VR significantly reduces pain and anxiety. |
|
15 |
Yentis SM,2006 |
Assessing regional blocks before caesarean section. |
|
the standardization is restricted to the stimulus, not to the way in which it is applied nor to the nature of the assessor’s questioning |
|
16 |
Patel R, et al,2022 |
Inadequate neuroaxial anesthesia in patients undergoing elective caesarean section:
|
Systematic review |
Spinal/combined spinal-epidural anesthesia was associated with a lower overall prevalence of inadequate neuroaxial anesthesia than epidural anesthesia |
|
17 |
Nor NM, et al,2013 |
Assessing blocks after spinal anesthesia for elective caesarean section: how different questions affect findings from the same stimulus. |
|
When describing a sensory block, not only is it necessary to indicate the exact stimulus used, but it is important to define the actual question asked of the patient. |
|
18 |
Plaat F,2022 |
Pain during caesarean section: whose decision is it? Anesthesia. |
|
Hypnosis not reduce pain in patients undergoing WCP, but may be effective for decrease anxiety before procedure |
|
19 |
Brull SJ,et al,1991 |
Zones of differential sensory block during extradural anesthesia. |
|
Zones of differential sensory block developed within 5 min of extradural injection of local anesthetic, and persisted for the next 55 min. In all instances, PP extended more cephalad than LT, and TE extended above PP levels. |
Table 2. The studies included in the review for the guideline.
The results of the search engine, were filtered based on the interventions, outcome, data on population, and methodological quality. After extraction and filtering with a patient population and exclusion criteria’s were done, were appraised for quality and conclusion was made based on their level of evidence and grades of recommendations that adapted from oxford center for evidence based medicine.
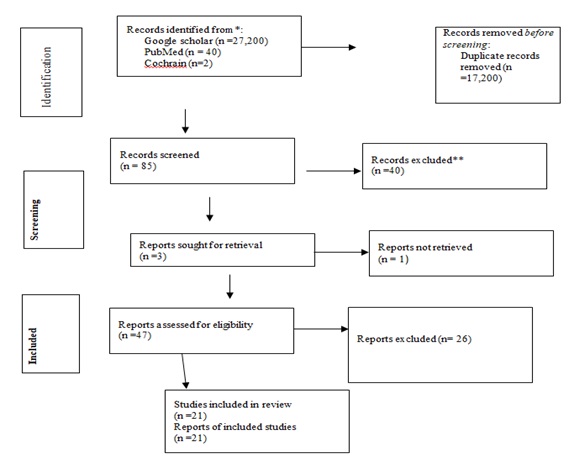 Figure 1. PRISMA Flow diagram of selection, screening and inclusion of studies.
Figure 1. PRISMA Flow diagram of selection, screening and inclusion of studies.
Inclusion criteria
Articles involving the management of failed spinal anesthesia during elective or emergency cesarean section with relevant outcomes were included.
Exclusion criteria
Articles without relevant outcomes,
ASA III and above,
Pregnant women developing high or total spinal anesthesia were excluded.
Definition, incidence and risk-factors for inadequate neuroaxial anesthesia
Depending on the definition, neuroaxial technique, and urgency of the caesarean section, there are different incidences of insufficient neuroaxial anesthetic. The term "failure" might refer to completely no blocks (no obvious sensory block), partial blocks (such as a unilateral block or an inadequate block height), the use of adjuvants, or the need to switch to general anesthesia [9].
Compared to epidural anesthesia, spinal anesthesia begins more quickly, has fewer problems, and requires less intraoperative supplementation. Kinsell a determined that the rates of failure to achieve a pain-free operation were 6% with spinal anesthesia, 24% with epidural top-up, and 18% with combined spinal-epidural anesthesia in a prospective audit of 5080 caesarean sections from a single facility [9].
Diverging opinions on the acceptable conversion rates of neuroaxial anesthesia to general anesthesia for emergency caesarean sections, particularly in time-sensitive circumstances, provide as an example of the challenges surrounding the definition of "failure." The Royal College of Anesthetists advises counting the use of general anesthesia as a converted neuroaxial method rather than main general anesthesia when it is administered alongside a labour epidural that is not topped up [10].
It is not surprising that the proportion of cases needing category-1 caesarean sections was higher when there was no attempt to top-up an indwelling epidural. Depending on how failure is defined, risk factors for insufficient neuraxial block can be identified. In his case series, Kinsella defined "failure" as either intraoperative discomfort caused by failure during surgery or preoperative failure to produce an adequate block. Operative urgency, higher BMI, first-time caesarean section mothers, and the criteria for caesarean section; acute fetal distress or a medical issue in the mother were all associated with pre-operative failure. The length of the procedure and the inadequacy of the pre-operative anesthetic block were important risk factors for intra-operative failure. The use of a spinal opioid decreased the risk of pre-operative failure when spinal anesthetic was utilized [9], LOC-4; GOR-C.
An increased number of boluses administered by a clinician during labor, the urgency of the caesarean section, and the provision of anesthesia services by a non-obstetric anesthetist were all identified as risk factors in a systematic review and meta-analysis of observational trials for unsuccessful conversion of labor epidural analgesia to caesarean section anesthesia [11], LOC-4; GOR-A.
A prospective study by Russell recorded levels of analgesia (loss of sensation of sharp needle pricks) and anesthesia (loss of tactile sensation) in 220 women undergoing caesarean section; there was no intraoperative pain [12-14], LOE – 2a and GOR – B. This suggests that loss of tactile sensation up to T5 is necessary to minimize the risk of pain during caesarean section, and this is widely confirmed. We included 70 women undergoing de novo epidural anesthesia (rarely used today) for incision, and none of the patients received axial opioids, so they are better than modern obstetric anesthesia practice.
The T5 dermatome is the putative target for acceptable block height in cesarean section, but several other factors add complexity to this seemingly simple standard. A key finding of Russell's study, which has been confirmed by other studies, is that axial anesthesia is associated with zones of differential sensory block at the cranial border [15,16]. Other studies have identified an inconsistent relationship between cold, sharp needle pricks and touch, which are used to assess neural axis block and the level of block. Therefore, one cannot be evaluated to predict the other [17,18]. Loss of cold sensation may be observed at levels several skin-tones above loss of sharp pinprick sensation, which may be several skin-tones above loss of touch sensation. Some authors found that sharp pinprick and cold scores were reversed, with much greater loss of sharp pinprick sensation than loss of cold sensation, but loss of tactile sensation was still the lowest. . None of the modalities change the effect from complete anesthesia to complete normal sensation within a single dermatome. For example, when using an ethyl chloride spray to assess cold block height, a woman may feel "cold" in one dermatome but "icy" in another. You may feel cold. There is no evidence as to what point between numbness and complete normal sensation represents the level of obstruction.
These difficulties are exacerbated by the lack of consensus on the stimuli that should be used to test sensory blocks. Kokarev et al. Different devices were used to assess block height after combined spinal epidural anesthesia in a group of women undergoing caesarean section [19], LOE – 1a and GOR – A. Six tests were used in random order to measure the four sensory modalities (Light touch). The light contact test spread the least on the skin, and the more expensive test offered no advantage over the cheapest test, cotton wool.
Nor and Russell studied the effect of using different questions to assess the same stimulus in a group of women undergoing caesarean section under spinal anesthesia [20]. The height of the block differed in her two dermatome medians depending on the question, suggesting that this is another variable to be defined. Finally, difficulties arise with the practical correlation of anatomical landmarks with specific dermatomes. Congreve et al. showed, in a study of 80 anesthetists of all grades, that one in seven were at least two dermatomes outside the‘correct’demarcation of T5 [21].
Most textbooks state that dense bilateral motor blocks of the lower extremities are essential. The inability to lift the leg against gravity indicates an L1-4 motor block, but does not reflect the density of the mid-upper chest block. The Bromage scale and some modifications have been used to describe the engine block [22,23], LOE – 1a and GOR – A.
An increasing proportion of anesthesiologists use the leg lift test to avoid confusion [24]. Evaluation of sympathetic block as part of overall block evaluation during axial anesthesia has received little attention. Lumbar axis anesthesia results in transient sympathectomy of the lumbar sympathetic chain and can be evidenced by the presence of warm, dry feet [25].
Since autonomic nerve fibers are most vulnerable to local anesthetics, unblocked sympathetic nerves suggest that sensory nerve fibers are less likely to be blocked [26]. A drop in blood pressure is not a sure sign of sympathetic block, as it can be caused by a variety of factors and masked by the use of vasopressor injections.
As pointed out, the dilemma of how to most effectively assess and ensure an acceptable nerve trunk block for cesarean delivery really made a big difference. The level of sensory block considered appropriate, how sensory block is tested, the reference point used, the blocked to unblocked or unblocked to blocked test. Whether or not to do so is also inconsistent. A survey of obstetric anesthesia practices published in 1997 found that 12% of his anesthesiologists did not regularly check upper levels for sensory block, and only 30% checked lower levels [27]. A comparison of practices in 2004 and 2010 showed that blocks from T4 to cooling remained the most commonly used standard for sensory blocks, but block height to light touch The number of evaluating anesthesiologists is also increasing [28].
Hoyle and Yentis conducted a literature review of methods to assess sensory and motor block (but not sympathetic block) in cesarean section under axial anesthesia from randomized clinical trials and recommendations from 45 editions of seven anesthesia textbooks [23]. They also found significant differences, but noticed over time a tendency to use a lighter touch to achieve T5 block height was not reported. When motor blocks were mentioned, less than half explained how they were actually used. When the method was specified, the majority mentioned the "Bromage scale", but only 5% of him agreed with Bromage's original description.
Seeking patient consent for neuroaxial anesthesia for caesarean section
A preoperative obstetric anesthesia consultation differs from other medical consultations in that women are more likely to undergo surgery for reasons other than their own health. In addition, limited time frames during emergencies make it difficult to share information and address women's specific concerns [29, 30]. This is another reason why every effort is made to anticipate emergencies in order to have appropriate conversations with women. This includes close cooperation between anesthesiologists, obstetricians and midwives and Communication is required [31]. There is evidence that neuroaxial anesthesia is only offered for caesarean anesthesia [32]. General anesthesia should be considered not only as a rescue technique but also as a major alternative to neuroaxial anesthesia.
While the administration of axial blocks may be routine for anesthesiologists, it should be borne in mind that axial blocks and caesarean sections are some of the important life events for women [33]. Her perception and reaction to the event depends on previous experience or lack thereof, (incorrect) information she may have received from other sources, and whether it is an emergency.
Assessing neuroaxial anesthesia for caesarean section
Currently, there is no single, widely accepted method for testing for a neural axis block prior to initiating a caesarean section. The block required for a caesarean section is the same as when using spinal or epidural anesthesia. However, spinal occlusion tends to be rapid, dense, and easy to assess. Multimodal testing should be used to assess the quality of the nerve axis block prior to initiation of surgery. Light touch sensory and motor blocks.
Assessment of sensory block Light touch should be used as the primary test method for targeting sensory block above T5. Sensory testing is essential, but we believe it is more error-prone than testing of other modalities because it relies on the woman's accurate interpretation of the anesthesiologist's questions. Performing sensory testing alone may increase the risk of intraoperative pain, especially if the language spoken by the anesthesiologist is not the woman's native language. When evaluating obstruction, it is important to give the woman enough time to respond. H. To avoid rapid movement along the dermatome. When ethyl chloride is used as an adjuvant, the accuracy of determining skin concentration may be affected by differences in spray distribution of different commercial formulations, which may cover multiple dermatomes [34].
Motor block assessment
The dense sensory block required for caesarean section is related to the dense motor block of the lumbosacral plexus. If the mother can raise a straight leg, the block is probably not suitable for caesarean anesthesia, no matter how severe the loss of sensation [35]. Complete motor block (plantar flexion) of S1 is characteristic of spinal anesthesia but is uncommon in epidural anesthesia. Normal ankle motor function during epidural anesthesia may indicate a lack of inadequacy of sacral anesthesia, which can cause pain during surgery.
Autonomic block assessment
Although it is the preferred strategy for determining block quality, there is no objective evidence that sympathetic nerve block should be part of the routine when evaluating sympathetic nerve block prior to caesarean section. However, it serves as an adjunct to sensory and motor testing to check for bilateral spread. A sympathetic block in the foot does not occur until a definite sensory block to T10 occurs. It can be assessed by feeling the temperature on both sides of the back of the toe. Differences in paw temperature or paw moisture indicate asymmetry or unilateral obstruction. Even if the sensory test shows no difference, the quality of the block on the cold side is probably not as good.
There is no evidence as to when or how often obstruction should be assessed after neuroaxial anesthesia. The time of onset depends on the nerve trunk technique and the drugs used [36], LOE – 1a and GOR – A.
Early evidence of some effect can increase patient confidence, but testing too early can be counterproductive. Testing a block multiple times can increase patient anxiety. After the test is repeated several times, the woman may feel pressure to say the block is working [33]. Before starting testing the block, it is important to reassure the woman that she is the best judge of the block and that everyone understands the importance of waiting until she is ready. It is described how to ask the surgeon to test the block with tweezers before performing the ablation, but the responsibility for block evaluation rests with the anesthesiologist.
It is essential that the assessment of the neuraxial block is comprehensively and accurately documented. This should include:
- The precise modalities that were used to test the block; the time of testing in relation to the administration of the neuraxial block or when the epidural top-up was completed
- When extension of labor epidural analgesia is used, the pre-operative block height should also be documented.
- Due to the variability in clinicians ‘interpretation of dermatomes, it has been suggested that the most reproducible way of documenting the height of the sensory block is using a dermatome map on the anesthetic chart or a similar.
Communication
In addition to the practical aspects of block assessment, it is important to consider communication between the anesthesiologist and the woman. A good relationship between the woman and the anesthesiologist can improve the accuracy of the sensory assessment. The sensory block test relies on the woman understanding what the anesthesiologist wants to know and being able to communicate what she is going through.
The reliability of the test will depend on the accuracy of a woman’s responses, which in turn can be affected by several factors, including:
Distress and distraction
The woman’s focus is the safe delivery of her baby. This may be overwhelming in emergencies where there are heightened concerns about the baby. This can include an inadequate neuraxial block in a previous pregnancy or domestic abuse (more common in pregnancy) [37], LOE – 2b and GOR – B.
Power of suggestion
It is essential to avoid what in a legal context would be called ‘leading the witness’, for example ‘I don’t think you can feel that?’. People can be vulnerable to suggestion, and this is increased by anxiety, distress and pain [31] Questions should be open and neutral.
Hierarchy
From necessity, women need to trust their anesthetist. The nature of the clinical situation means that it is unrealistic to expect the woman to behave as an ‘equal partner’ [33]. Although clinicians ‘confidence and professionalism are reassuring to patients, it is crucial to remain aware that they may also inhibit a woman from speaking out if she is concerned.
Time pressure
For anesthetists, a time-pressured environment is commonplace; it is easy to forget that this pressure will be obvious to the woman and can be intimidating.
Anaesthetic confirmation bias
On the vast majority of occasions, the block, especially if intrathecal, will be successful. Confirmation bias means the anesthetist may unwittingly pay attention to the information that fits prior experience. The anesthetist should make a conscious effort to look for signs of an inadequate block.
Managing pain and distress during caesarean section under neuroaxial anesthesia
For axial block inadequate for cesarean delivery, response is determined by the urgency of the cesarean section, the stage of cesarean section at which the woman experiences pain and discomfort, and the primary axial block procedure. Anesthesiologists must maintain situational awareness and be aware that a 'perfect' block can fail and no test is foolproof [38], LOE – 1a and GOR – A.
Similarly, the effectiveness of blockade may change over time during a caesarean section. Women are the primary source of information about block effectiveness and should be listened to carefully. Inadequate or delayed treatment, not necessarily failure of the nerve axis block, causes the greatest distress to patients [33-39]. When a clinician ignores a woman's experience, it increases her distress and can lead to trauma. Subjective childbirth experience is the strongest predictor of postnatal trauma [40, 41], LOE – 2b and GOR – B.
The anesthetist should establish the nature of the woman’s pain, reassure her that she is being heard and that they will endeavor to make her more comfortable. Appropriate support can offer the best prospect of mitigating the long-term adverse impacts of block failure.
Management will depend on the urgency of surgery, stage of procedure and severity of the pain
The following Nine ‘A’ steps should be taken:
- Acknowledge the patient’s distress and inform the operating theatre team.
- Ask the surgeon to stop surgery as soon as it is safe to dose. If the pain is severe and the woman’s and the baby’s lives are not in danger, surgery should immediately behalted, except between uterine incision and delivery. If atthis stage, the obstetrician should be asked to achieve delivery as quickly as possible.
- Reassure the woman (and her partner) that you will manage the pain.
- If pain occurs early on, especially before delivery, analgesic adjuvants are unlikely to be fully effective. If the urgency of surgery permits, consideration should be given to a second neuraxial technique (in the case of spinal anesthesia) or extending the neuraxial technique(in the case of combined spinal–epidural or epidural extension anesthesia). If these options are not possible, general anesthesia should be recommended.
- Do not treat pain with anxiolytics.
- If there is an indwelling epidural catheter and time, check the block. Additional top-ups could be considered. Alkalinised lidocaine with adrenaline is likely to achieve the most rapid effect. Do not allow surgery to restart without re-checking the block.
- Ask the surgeon to try to minimize surgical stimuli, for example exteriorization of the uterus is not recommended because it is associated with a higher incidence of intra-operative nausea and vomiting, increased postoperative pain and does not improve operative outcomes such as hemorrhage and infection [42], LOE - 1a and GOR - A.
- Make a detailed record of events on the anesthetic chart. Include what treatment was offered, the patient’s response and any recommendation of general anesthesia.
- If other strategies have failed and the woman requests it, provide general anesthesia.
The anesthetist should use their knowledge and expertise to decide when general anesthesia should be offered and when it should be recommended. The woman should, if possible, be included in the discussion about how to proceed.
Follow-up for women who experience pain and distress during caesarean section under neuroaxial anesthesia.
Follow-up is essential to minimize the development of long-term psychological sequelae [40].Ensure that all persons caring for the woman before and after discharge are aware of intraoperative events. Follow-up should be prompt and, if possible, carried out by the anesthesiologist who supervised it (in the case of a trainee anesthesiologist, he should be assisted by an experienced colleague). In some cases, women may feel unable to see the same anesthesiologist and an experienced colleague should fill the role instead. A woman needs to be listened to and her account of events needs to be accepted as her actual experience.
Education about possible reasons for intraoperative pain should be provided. Any questions or concerns a woman may have should be addressed as fully as possible. If the woman remains distressed, further follow-up with senior staff may be appropriate. Lack of or indifference to postoperative care can exacerbate long-term psychological effects. The report should be sent to the woman's primary care physician and city midwifery services. If concerns persist, advise the woman to contact an anesthesiologist so that assistance can be obtained if needed. Women may be late in reporting pain during surgery. Questions can only be asked if she is pregnant again.
All women should be informed that they can request an appointment with an anesthesiologist to confirm the event and plan anesthesia management for their next birth.
Application of these guidelines in resource-limited settings
The principles outlined in these guidelines are applicable and accessible even in resource-constrained environments. Concerns about improper spinal blocks are relevant in any situation. However, contextual factors can influence local practice and make it difficult to achieve the same standards in different [43]. Clinical settings. Literally, in many countries there is limited resources, as also opioids suitable for neuroaxial anesthesia are not available. As a result, spinal and epidural anesthesia rely primarily on local anesthetics, are more prone to intraoperative pain, and require more tight blocks. Maternal mortality can be 50 times higher in resource-constrained settings than in high-income countries [44], LOE – 2b and GOR – B.
Anesthesia contributes disproportionately to this mortality rate. Her 1 in 7 deaths are due to anesthesia in resource-limited settings [45], LOE - 1a and GOR – A. Therefore, maternal discomfort during caesarean delivery may be perceived as a minor consequence. In some areas, an anesthesiologist must perform both surgery and anesthesia (in South Africa, up to 7% of maternal deaths were caesarean sections by her one physician) [46]. These factors make pain management difficult and reduce the level of attention a physician can provide. Anesthesia providers are often inexperienced and unqualified. In some areas, she is the only anesthesiologist for every million women [47], LOE - 1a and GOR - A.
Exposure to general anesthesia and non-physician anesthesiologists is associated with increased risk for mothers in low- and middle-income countries. Increased risks from general anesthesia may be related to poor maternal health (e.g., obstetric bleeding), but South Africa reported that 10 of 92 deaths were due to inadequate spinal block were under anesthesia during general anesthesia by [48]. Therefore, given the maternal risk in the hands of inexperienced anesthesia providers, there may be reluctance to convert failed spinal blocks to general anesthesia.
There are scant statistics on the frequency of botched spinal procedures in resource-constrained settings, although they are likely to be higher than the 1 in 10 cases reported in a single study [49]. According to a South African study, only 56% of anesthetic companies manually assess the spinal block [50]. Furthermore, there hasn't been agreement on the best way to check the block or the appropriate block height. On-professional anesthetists had been significantly more likely to replicate the spinal and much less likely to transform to modern anesthesia in response to an inadequate block. Despite the fact that more than 95% of respondents expected to be able to provide modern anesthetic for caesarean sections, more than a third thought they were no longer able to do so.
These criteria imply that in settings with limited resources, appropriate pre-operative counseling and spinal block assessment are crucial. When there are language hurdles, innovative methods like information movies on smartphones may reduce anxiety and guarantee the mother receives the information in her first language consistently [51]. Although the tolerable threshold of pain needing conversion to general anesthetic may need to be evaluated against the associated maternal risk in resource-constrained settings, the management of pain following caesarean section follows similar concepts to those indicated in these guidelines. The use of local anesthetic infiltration by the surgeon, in addition to the previously stated methods, may prove useful in delivering safe and efficient supplemental analgesia. The answer ultimately lies in a thorough evaluation of the block prior to the incision.
Conclusion and Recommendations
A woman who experiences pain during caesarean section under neuroaxial anesthesia is at risk of adverse psychological sequelae. Litigation arising from pain during caesarean section under neuroaxial anesthesia has replaced accidental awareness under general anesthesia as the most common successful medicolegal claim against obstetric anesthetists.
Recommendations
General anesthesia and neuroaxial procedures must be explained in order to obtain informed permission for caesarean section anesthesia.
Discuss the intended amount of block and how it will be assessed for neuroaxial techniques, the sensations to be anticipated with an effective block, the likelihood of pain, and potential pain treatments, including general anesthesia.
For non-elective caesarean sections, consideration should include potential fetal risks arising from the time it takes to provide a viable method of anesthesia.
Use established techniques for nerve trunk block in cesarean delivery with sufficient doses of local anesthetic and opioids.
Using light touch as the primary testing method, we aim for sensory blocks up to T5 and above. If the degree of obstruction is in doubt, a second confirmatory sensory modality should be used.
Identify the blocking plane as the point where sensation is first felt when switching bilaterally from the blocked dermatome to the unblocked dermatome between the midaxillary and midclavicular lines.
Test the bottom and top edges of the block and use the back of the leg if necessary to avoid spraying near the genital area.
Also, use straight-leg raises as a simple, reproducible test for motor block. Effective blocking is indicated by the inability to lift straight legs to the sides against gravity.
After acknowledging complaints of pain and stress and asking the surgeon to stop treatment when it is safe to do so, give fast-acting opioids or intravenous ketamine first as shown by (Figure 2).
If possible, requests for general anesthesia should be granted. It is good practice for anesthesiologists to recommend general anesthesia when other methods are unlikely to provide effective analgesia.
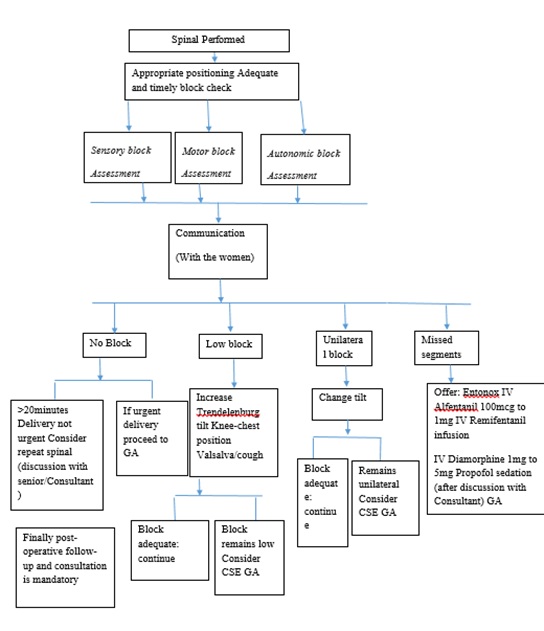 Figure 2: Management of failed or inadequate Spinal Anesthesia in obstetric clients.
Figure 2: Management of failed or inadequate Spinal Anesthesia in obstetric clients.
Ethics approval and consent to participate
Not applicable
Author’s contributions
The corresponding author and Meku Tade had contributes in the study by conceptualization, investigation, methodology, supervision, validation and writing and editing the review. Mengistu Yinges, Kidanemariam Tamrat, and Gudeta Teku had made a contribution in conceptualization, investigation, methodology, formal analysis, validation and writing draft, and final selection of the journal.
Availability of data and materials
Data are available with the corresponding author’s address upon reasonable request.
Funding
No funding was sought
Competing interest
No competing interest in this work.
Acknowledgments
We would like to thanks all authors who play a great contribution to the base line finding to our study.
References
- Olawin AM, Das JM (2022) Spinal Anesthesia In: Stat Pearls [Internet]. Treasure Island (FL): StatPearls Publishing
- Guidelines for Management of Inadequate Regional Block for Caesarean Section
- Abraham AA, Philip J (2013) Failed spinal anesthesia- management by giving a second spinal, Sri Lankan. J Anesthesia 21: 14-19.
- Simeen M, Jamal, Jameel S, Sirajuddin M (2017) An observational prospective cohort study of incidence of spinal failure and Need of Supplement 16: 75-77.
- Yentis SM (2006) Height of confusion: Assessing regional blocks before caesarean section. International Journal of ObstetricAnesthesia 15: 2-6.
- Patel R, Kua J, Sharawi N, Bauer ME, Blake L, et al. (2022) Inadequate neuroaxial anesthesia in patients undergoing elective caesarean section: A systematicreview.Anaestheia 77: 598-604.
- Nor NM, Russell IF (2013) Assessing blocks after spinal anesthesia for elective caesarean section: How different questions affect findings from the same stimulus. Int J Obstet Anesth 22: 294-297.
- Plaat F (2022) Pain during caesarean section: whose decision is it? Anesthesia 77: 941.
- Kinsella SM (2008) A prospective audit of regional anesthesia failure in 5080 caesarean sections. Anaesthesia 63: 822-832.
- https://www.rcoa.ac.uk/sites/default/files/documents/2019-09/CSQ-ARB-2012_0.pdf
- Bauer ME, Kountanis JA, Tsen LC, Greenfield ML, Mhyre JM (2012) Risk factors for failed conversion of labor epidural analgesia to cesarean delivery anesthesia: A systematic review and meta-analysis of observational trials. International Journal of ObstetricAnesthesia 21: 294-309.
- Gasner A, Aatsha PA (2021) Physiology, Uterus Stat Pearls.
- Sharabi AF, Lui F.Anatomy (2022) Abdomen and Pelvis, SplanchnicNerves. Stat Pearls.
- Russell IF (1995) Levels of anesthesia and intraoperative pain at caesarean section under regional block. International Journal of Obstetric Anesthesia 4: 71-77.
- Brull SJ, Greene NM (1989) Time-courses of zones of differential sensory blockade during spinal anesthesia with hyper baric tetracaine or bupivacaine. Anesthesia and Analgesia 69: 342-347.
- Brull SJ, Greene NM (1991) Zones of differential sensory block during extra-dural anesthesia. British Journal of Anaesthesia 66: 651-655.
- Ousley R, Egan C, Dowling K, Cyna AM (2012) Assessment of block height for satisfactory spinal anesthesia for caesarean section. Anaesthesia 67: 1356-1363.
- Russell IF (2004) A comparison of cold, pinprick and touch for assessing the level of spinal block at caesarean section. International Journal of Obstetric Anesthesia 13: 146-152.
- Kocarev M, Watkins E, McLure H, Columb M, Lyons G (2010) Sensory testing of spinal anesthesia for caesarean section: Differential block and variability. International Journal of Obstetric Anesthesia 19: 261-265.
- Nor NM, Russell IF (2013) Assessing blocks after spinal anesthesia for elective caesarean section: How different questions affect findings from the same stimulus. International Journal of Obstetric Anesthesia 22: 294-297.
- Congreve K, Gardner I, Laxton C, Scrutton M (2006) Where is T5? A survey of anaesthetists. Anaesthesia 61: 453-455.
- Bromage PR (1965) A comparison of the hydrochloride and carbon dioxide salts of lidocaine and prilocaine in epidural analgesia. Act a Anaesthesiologica Scandinavica 9: 55-69.
- Hoyle J, Yentis SM (2015) Assessing the height of block for caesarean section over the past three decades: Trends from the literature. Anaesthesia 70: 421-428.
- Yentis SM, Lucas DN, Brigante L (2020) Safety guideline: Neurological monitoring associated with obstetric neuroaxial block 2020: A joint guideline by the Association of Anesthetists and the Obstetric Anaesthetists’Association. Anaesthesia 75: 913-919.
- Laishley RS, Morgan BM (1988) A single dose epidural technique for caesarean section. A comparison between 0.5% bupivacaine plain and 0.5% bupivacaine with adrenaline. Anaesthesia 43: 100-103.
- Rocco AG, Raymond SA, Murray E, Dhingra U, Freiberger D (1985) Differential spread of blockade of touch, cold, and pinprick during spinal anesthesia. Anesthesia and Analgesia 64: 917-923.
- Bourne TM, DeMelo AE, Bastian pillai BA, May AE (1997) A survey of how British obstetric anesthetists test regional anesthesia before caesarean section. Anaesthesia 52: 901-913.
- Husain T, Liu YM, Fernando R (2013) How UK obstetric anesthetists assess neuroaxial anesthesia for caesarean delivery: National surveys of practice conducted in 2004 and 2010. International Journal of Obstetric Anesthesia 22: 298-302.
- Fortescue C, Wee MYK, Malhotra S, Yentis SM, Holdcroft A (2007) Is preparation for emergency obstetric anesthesia adequate? A maternal questionnaire survey. International Journal of Obstetric Anesthesia 16: 336-340.
- Carvalho B, Cohen SE, Lipman SS, Fuller A, Mathusamy AD, et al. (2005) Patient preferences for anesthesia outcomes associated with cesarean delivery. Anesthesia and Analgesia 101: 1182-1187.
- Brinkler R, Edwards Z, Abid S, Oliver CM, Lo Q, et al. (2019) A survey of antenatal and peripartum provision of information on analgesia and anaesthesia. Anaesthesia 74: 1101-1111.
- Clayton MA, May RL, Lucas DN, Richardson AL (2020) Anesthetic consent for elective caesarean section. International Journal of Obstetric Anesthesia S16: P81.
- Stanford SER, Bogod DG (2016) Failure of communication: A patient’s story. International Journal of Obstetric Anesthesia 28: 70-75.
- Harty ECB, Bopitiya P, Bogod D, Lucas DN (2019) An assessment of the distribution of different ethyl chloride sprays. International Journal of Obstetric Anesthesia S15: P5.
- Collis R, Harries S, Theron A (2020) Obstetric Anesthesia (Oxford Specialist Handbooks in Anesthesia). 2nd ed. Oxford: Oxford University Press 2020.
- Reschke MM, Monks DT, Varaday SS, Ginosar Y, Palanisamy A, et al. (2020) Choice of local anesthetic for epidural caesarean section: A Bayesian network meta-analysis.Anaesthesia 75: 674-682.
- Finnbogadottir H, Dykes AK (2016) Increasing prevalence and incidence of domestic violence during the pregnancy and one and a half year postpartum, as well as risk factors:- A longitudinal cohort study in southern Sweden. BMC Pregnancy andChildbirth 16: 327.
- Fettes PDW, Jansson JR, Wildsmith JAW (2009) Failed spinal anesthesia: Mechanisms, management, and prevention. British Journal of Anaesthesia 102: 739-748.
- Harris R, Ayers S (2012) What makes labour and birth traumatic? A survey of intrapartum ‘hotspots’. Psychology and Health 27: 1166-1177.
- Vogel TM, Homitsky S (2020) Antepartum and intrapartum risk factors and the impact of PTSD on mother and child. British Journal of Anesthesia Education 20: 89-95.
- Garthus-Niegel S, von Soest T, Vollrath ME, Eberhard-Gran M (2013) The impact of subjective birth experiences on post-traumatic stress symptoms: A longitudinal study. Archives of Women’s Mental Health 16:1-10.
- Sen TH, Taylor CR, Sharawi N, Sultana R, Barton KD, et al. (2022) Uterine exteriorization versus in situ repair in cesarean delivery: A systematic review and meta-analysis. Can J of Anesth 69: 216-233.
- Royal College of Anesthetists/Association of Anaesthetists. NAP5 Anesthesia Awareness Support Pack. 2014.
- Bishop D, Dyer RA, Maswime S, van Dyk D, Kluyts HL, et al. (2019) Maternal and neonatal outcomes after caesarean delivery in the African surgical outcomes study: A 7-day prospective observational cohortstudy. Lancet Global Health 7: 513-522.
- Sobhy S, Zamora J, Dharma rajah K, Arroyo-Manzano D, Wilson M, et al. (2016) Anesthesia-related maternal mortality in low-income and middle-income countries: A systematic review and meta-analysis. Lancet GlobalHealth 4: e320-327.
- Gebhardt GS, Fawcus S, Moodley J, Farina Z (2015) Maternal death and caesarean section in South Africa: Results from the 2011–2013 saving mothers’ report of the National Committee for confidential enquiries into maternal deaths. South African Medical Journal 105: 287.
- Hoyler M, Finlayson SRG, McClain CD, Meara JG, Hagander (2014) Shortage of doctors, shortage of data: A review of the global surgery, obstetrics, and anesthesia workforce literature. World Journal of Surgery 38: 269-280.
- Moodley J, Pattinson RC, Fawcus S, Schoon MG, Moran N, et al. (2014) The confidential enquiry into maternal deaths in South Africa: A case study. British Journal of Obstetrics andGynaecology 121: 53-60.
- Rukewe A, Adebayo OK, Fatiregun AA (2015) Failed obstetric spinal anesthesia in a Nigerian teaching hospital: Incidence and risk factors. Anesthesia and Analgesia 121: 1301-1305.
- Jones GW, Samuel RA, Biccard BM (2017) Management of failed spinal anesthesia for caesarean section. South African Medical Journal 107: 611-614.
- Purcell-Jones JMA, Haasbroek M, Van der Westhuizen JL, Dyer RA, Lombard CJ (2019) Overcoming language barriers using an information video on spinal anesthesia for cesarean delivery: Implementation and impact on maternal anxiety. Anesthesia and Analgesia129: 1137-1143.
Citation: Ilala TT, Ayano GT, Kebede MY, Yilma KT, Tade M (2023) Evidence-based practical Guideline on the Management of Failed Spinal Anesthesia in pregnant mothers undergoing Caesarean Section in a Resource constrained area; Systematic Review Article. J Anesth Clin Care: 10: 078.
Copyright: © 2023 Tajera Tageza Ilala, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

