
Interventions for Mental Health Care in Gestation and Puerperium Review
*Corresponding Author(s):
Matilde Fernández Y Fernández-ArroyoMadrid Health Service (SERMAS), Primary Care, Barrio Del Pilar Health Centre, Spain
Email:mfernandezarroyo@gmail.com
Abstract
Introduction: The foundations of a person's health are intimately related to physical and psychological maternal health. Physical care is protocolised and rapidly disseminated throughout the health care However, psycho-emotional care of pregnant and postpartum women receives less attention.
Objective: To describe psycho-emotional care interventions during pregnancy and the postpartum period.
Methodology: Literature review in the following databases: PubMed, Cumulative Index in Nursing and Allied Health Literature (CINAHL) Cochrane Library. The search for scientific articles was carried out in English and Spanish. The selected keywords used were "pregnancy", "postpartum", "mental health" and prevention strategies". After several analysis processes, the most relevant papers were selected.
Results: Eight pillars of gestational and postpartum care that affect maternal and newborn health emerged from the literature review: diet, micronutrient supply, exercise, toxics, pathogens, cognitive-behavioural strategies, history of mental health disturbance, interpersonal violence.
Discussion: All psycho-emotional care interventions during pregnancy and the postpartum period have an impact on perinatal health. The paper provides a well-founded explanation for professionals to understand the impact of psycho emotional care on the health of women and newborns in these periods.
Keywords
Mental Health; Postpartum Pregnancy; Prevention Strategies
Introduction
Epigenetic advances provide evidence that the foundations of human health are intimately related to maternal health in gestation [1]. Individuals exposed to stress early in life are more likely to suffer long-term behavioural, mental health, metabolic, immune and cardiovascular consequences [2]. The hypothalamus plays a nodal role in programming, controlling and regulating stress responses throughout the life course [3]. Epigenetic reprogramming in the hippocampus and hypothalamus plays an important role in adapting genome function to experiences and exposures during the perinatal and early life periods and in establishing stable phenotypic outcomes [4]. The World Health Organization (WHO) states that nutrition, weight control, physical activity, pregnancy planning, as well as the physical, mental and psychosocial health of the pregnant woman are priorities to ensure the health of the future child [5-7]. Progress in understanding how a mother's emotional states during pregnancy affect the health of her unborn child has been less well established scientifically, but there is now compelling evidence that this is beginning to emerge. Current data show that maternal mental conditions affect about 10% of pregnant women worldwide. Therefore, assessing the timing and patterns of mental health illnesses is critical to ensure the well-being of the mother, the newborn and the whole family [8]. Pregnancy is a time of increased risk of developing or re-experiencing mental illness [9]. Women with previous mental health conditions may increase the risk of miscarriage and other pregnancy complications (e.g. gestational diabetes), premature birth and low birth weight [10]. Gestational healthcare needs to take into account advances in antenatal psychology.
Objective
To describe interventions for mental health care in pregnancy and the postpartum period.
Methodology
A literature review was conducted in the following databases: PubMed, Cumulative Index in Nursing and Allied Health Literature (CINAHL Cochrane Library. The search for scientific articles was carried out in English and Spanish. The keywords used were selected through the Medical Subject Headings (MeSH) and Health Sciences Descriptors (DeCS) terms. The terms were "pregnancy", "postpartum", "mental health", "prevention strategies". The search was carried out using the Boolean operator "AND". The Boolean combinations used were: "mental health AND prevention strategies AND pregnancy"; "mental health AND prevention strategies AND postpartum"; "pregnancy AND mental health"; "postpartum AND mental health". The initial search yielded a total of 14,499 articles. In order to refine and fulfil the research objective, several inclusion criteria were applied that helped to reduce the sample obtained: scientific articles published from 2018 to 2022; open access articles; qualitative, quantitative and mixed methodological designs; works whose central dimension was the prevention of mental health in pregnancy and postpartum. After applying the above criteria, a total of 506 articles were obtained. The third stage of the study involved the elimination of articles that were repeated in the 3 databases, studies that were opinion columns or recommendations, studies that were not published in the three databases. The third stage of the study involved the elimination of articles that were repeated in the 3 databases, studies that were opinion columns or general recommendations on gestational or postpartum care, articles that reflected studies on pathologies prior to gestation or in relation to pregnancies with assisted reproduction techniques. Finally, after the third stage of selection, a total of 20 scientific articles were obtained, which are presented in the bibliography, from which two analytical categories emerged and which are developed in the results section (Figure 1).
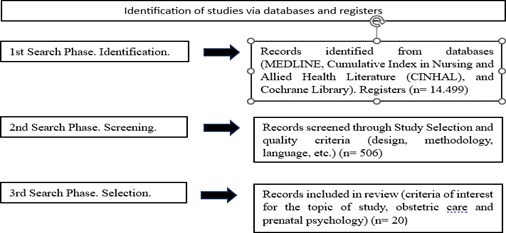 Figure 1: Flow diagram literature search strategy.
Figure 1: Flow diagram literature search strategy.
Results
Eight pillars of gestational and postpartum care that affect maternal and newborn health emerged from the literature review: diet, micronutrient supply, exercise, toxics, pathogens, cognitive-behavioural strategies, history of mental health disturbance, interpersonal violence.
Diet
Studies show a direct relationship between pre-pregnancy body mass index and increased adverse perinatal outcomes [6]. Poor maternal nutritional status is associated with abnormal fetal growth patterns, including low birth weight (<2500 g), small for gestational age (<10% of birth weight for gestational age) or fetal growth restriction. Maternal obesity is associated with macrosomia (>4 to 4.5 kg) and large for gestational age (>90 % of birth weight for gestational age), gestational diabetes mellitus (GDM) and pre-eclampsia. All disorders are associated with an increased risk of developing chronic diseases in childhood and adulthood [11]. Persistent very high fetal glucose concentrations can inhibit fetal neuronal development, leading to reduced neuronal number, dendritic proliferation and synapse formation, leading to reduced cognitive function and increased developmental learning difficulties [12]. GDM is associated with neurodevelopmental disorders: autism spectrum disorder (ASD) (RR=1.28, Arango) [13]; and attention deficit hyperactivity disorder (ADHD) [14] (OR=1.63, Arango) (13). Arango et al. (2021) find diabetes mellitus type 2 (hazard ratio, RR 1.54 to 2.28), depression (RR 1.65 to 1.99) and low frequency of social contacts (RR=1.57) as risk factors for dementia [13]. Observational data have shown that first trimester gain is the strongest predictor of adverse outcomes [11].
Micronutrient supply
Micronutrients are minerals and vitamins necessary for the normal growth and development of living organisms [15]. Their inadequate intake can lead to deficiencies in maternal reserves, microbiota alteration, maternal diseases, fetal and neonatal developmental pathology [6]. Folic acid is recommended for the prevention of neural tube defects. Supplementation with 400 mcg/d of folic acid is recommended from 3 months before conception, during pregnancy and up to 4-6 weeks postpartum or for the duration of breastfeeding [5,16]. Iodine is an essential nutrient for making thyroid hormones, which are essential for regulating the development of the fetal brain and nervous system. Nervous tissue begins to develop as early as the second month of pregnancy [17]. Altered iron status during pregnancy can result in anaemia, fatigue, preterm birth, low birth weight and increased perinatal mortality. The recommended daily intake during pregnancy is 27-28 mg/d [18]. Calcium is essential for bone formation, muscle contraction, enzyme and hormone function. During pregnancy, it is necessary to maintain an intake of 1,000-1,200 mg/d [18]. Calcium intake has been associated with a reduced risk of pre-eclampsia (RR: 0.38; 95% CI: 0.28-0.52; 9 studies), hypertension (RR: 0.53; 95% CI: 0.38-0.74; 5 studies) prematurity in all women (RR: 0.76; 95% CI: 0.66-0.97) [18]. Vitamin D is related to bone health and has an immunological and anti-inflammatory role. Deficiency in pregnancy is associated with an increased risk of developing GDM, pre-eclampsia, prematurity and low birth weight [19]. Vitamin C is necessary during embryonic development for several epigenetic enzymes to be active and involved in cell differentiation, maintenance of pluripotency and developmental functions [18,20]. Prebiotics and probiotics in pregnancy are suggested for their role in the remodelling of metabolic pathways. There is weak evidence of their adverse impact on foetal development [18,21].
Exercise
Moderate physical activity during pregnancy improves muscle tone and function and decreases the risk of pre-eclampsia, gestational diabetes and overweight. Studies claim that an average of 30 minutes of exercise per day contributes to long-term benefits for maternal health [6].Exercise improves metabolic homeostasis and muscle-based thermogenesis in the foetus and offspring by inducing the function of apelin exerkinin in foetal muscle [22,23]. Apelin is an exercise-induced myokine that can enhance maternal and fetal muscle cell metabolism that has beneficial metabolic effects by reducing obesity-related insulin resistance [22]. Arango found exercise to be a robust protective factor for Alzheimer's disease (hazard ratio, HR=0.62) [13].
Toxics
Exposure to toxic substances has a direct impact on maternal and neonatal morbidity and mortality [13]. Alcohol is a teratogen that can easily cross the placenta and damage the developing embryo and foetus because it has a prolonged effect due to amniotic accumulation, increasing the risk of negative outcomes, including foetal alcohol spectrum disorder [24,25]. Smoking during pregnancy is associated with reduced fetal measurements after the first trimester [26]. Arango found associations between gestational smoking with attention deficit hyperactivity disorder (OR=1.60) with opioid use disorders (odds ratio, OR=3.07) [13]. The effects of drugs administered to pregnant women are less well known because the biochemical and physiological changes of pregnancy alter the dose-response relationship. The lack of evidence recommends individualised assessment [27,28]. Cannabis (marijuana) use has the potential to cause adverse foetal and infant development. Exposed children have lower scores on tests of visual problem solving, visual-motor coordination, visual analysis, decreased attention span and more behavioural problems [29]. Arango also found an association with non-organic psychotic disorders (OR=3.90) [13]. There is no safe amount of marijuana during pregnancy and lactation [29]. Toxic metals and endocrine disruptors are pollutants that are ubiquitous in the environment. Many metals, such as Arsenic (As), Cadmium (Cd), Lead (Pb) and Mercury (Hg), cross the placental barrier resulting in direct foetal exposure [30]. Prenatal exposure results in fetal epigenomic changes, including altered global DNA methylation and microRNA expression. These changes may have functional cellular consequences, which will affect the future health of the child [30].
Pathogens
The classical infectious pathogens: toxoplasma gondii, rubella virus, cytomegalovirus herpes simplex virus (TORCH), are teratogenic. Emerging evidence suggests that these infections represent the extreme end of a much broader spectrum of lesions that may alter fetal brain development, leading to future neuropsychiatric consequences for the child [4]. The link between influenza infections in pregnant women and an increased risk of developing schizophrenia in their children was first described more than 30 years ago. Since then, it has been found that a variety of infections during pregnancy can increase the risk of autism spectrum disorder and depression in the child. Both infections and inflammation can cause direct injury to neurons and neural progenitor cells or indirect injury through activation of microglia and astrocytes, which can trigger cytokine production and oxidative stress [7]. They can also alter serotonin production in the placenta, which can disrupt neurotransmitter signaling in the developing brain [4].
Cognitive-Behavioural Strategies
Prenatal and postnatal education programmes have shown their impact on women's health in these periods in terms of gestational care, nutrition, exercise, breathing techniques, relaxation, childbirth care, bonding with the baby, family reorganization, breastfeeding and infant care [6,31,32,33,34,35].
History of Mental Health Disturbance
Pregnancy involves psychological and social processes that have an impact on the neurological development of the newborn [10,36,37]. Pregnancy is a time of increased risk of developing or re-experiencing mental illness [9]. In the case of depression, the average prevalence of maternal depression ranges from 15.6% in the antenatal period to 19.8% in the postnatal period. It is associated with preterm birth, low birth weight and poor infant growth and cognitive development [31,38,39]. Worldwide, suicide is one of the leading causes of maternal mortality. Figures range from 13.4% in France to 11% in the USA. Psychiatric history was found in 33.3% of suicidal mothers in France and depression in 75% of those in the USA. The history was found to be unknown to the maternity team for 30.3 % in France. Ninety-one percent of potentially preventable maternal deaths were related to lack of multidisciplinary management and/or inadequate interaction between the patient and the health system [40,41,42].
Interpersonal Violence
Interpersonal violence in the perinatal period is a prominent health problem because of the risk of escalation of violence and the significant impact on mothers' parenting after childbirth [43]. It can be associated with fatal and non-fatal adverse health outcomes due to direct trauma to a pregnant woman's body and the effect of stress on foetal growth and development. Emotional violence is a risk factor for prenatal and/or postpartum depression and mother-child bonding [44].
Discussion
The results show a high degree of evidence on the five pillars of perinatal health, diet, micronutrient intake, exercise, toxic reduction and infection control. These five pillars are crucial because of their direct impact on the health of the pregnant woman and foetal development [35]. However, a great disparity of criteria for recommendations has been found in the main international health and scientific organizations (WHO, NICE; FIGO, etc.) [5,10,15,16]. This lack of consensus hinders the proper management of care interventions for pregnant women and early detection of perinatal health problems and more seriously, the development of institutional policies that effectively organise prenatal care [45]. Observational data have shown that first trimester care is the strongest predictor of adverse outcomes. Interventions starting early in pregnancy or before conception are needed to prevent later complications for mothers and their children [11]. Cognitive behavioural strategies have been found to be developed through maternal and paternal health education programmes in gestation and the postpartum period [46]. There is evidence of their usefulness in favouring a healthy pregnancy, delivery and puerperium, with a satisfactory experience and lower risks of maternal and neonatal morbidity and mortality [34]. However, it is difficult to know which schools have the greatest capacity to achieve the educational objectives and, therefore, which schools should be extended throughout the world. Their study is limited by the heterogeneity of evaluation designs [35]. With regard to the mental health of pregnant and puerperal women, the evidence shows that there are very high percentages of women with mental health problems that go unnoticed by the health teams that care for them during pregnancy and the puerperium [42]. We agree with Blackmore's team [9] on the need to incorporate perinatal mental health screening tools for all pregnant women into national programmes. Strategies must be designed to overcome individual and health system barriers to implementing policies for early detection of perinatal mental health. Montagnoli's recommendation [8] for prevention and management of maternal mental health conditions within the first 1000 days with a holistic approach is highlighted. The lack of prenatal psychology teams hinders this task of holistic care. Recommendations from state maternal mortality review committees can be useful in prioritising interventions and strategies to enable screening, care coordination and continuity of care during pregnancy and the postpartum year [41,42]. The contribution of Alberdice [33] on the role of midwives in the prevention of maternal mental health and detection of domestic violence is very interesting, given their role in accompanying women and their partners throughout the process of pregnancy, childbirth and the postpartum period. Blackmore [9] proposes training health professionals and implementing digital screening. According to Jardin, the training of health professionals should include sexual and reproductive rights issues [47]. The main limitation of the paper lies in its review format conducted in biomedical databases. One wonders what the results would be in psychological databases. However, this is also its greatest value, as it provides a very broad view of what is seen as prenatal psychology prevention from a health perspective. The study highlights the need for training of health professionals in this area and the need to establish prenatal psychology teams that coordinate with obstetric teams to ensure comprehensive care for women in these vulnerable stages of life, gestation and puerperium. It may also represent a benchmark for advancing clinical characterisation and research and for expanding preventive and early intervention strategies for mental disorders.
Acknowledgment
World Association for Infant Mental Health (WAIMH) and CONECTA PERINATAL and ASMI WAIMH-Spain. Who have commissioned this work for the European-Latin American Congress, 16-18 February 2023.
References
- Davies C, Segre G, Estradé A, Radua J, De Micheli, et al. (2020) Prenatal and perinatal risk and protective factors for psychosis: a systematic review and meta-analysis. The lancet. Psychiatry 7: 399-410.
- Cao-Lei L, de Rooij SR, King S, Matthews SG, Metz GAS, Roseboom TJ et al. (2020) Prenatal stress and epigenetics. Neuroscience and biobehavioral reviews 117: 198-210.
- Uccellini O, Benlodi A, Caroppo E, Cena L, Esposito G, et al. (2022) 1000 Days: The "WeCare Generation" Program-The Ultimate Model for Improving Human Mental Health and Economics: The Study Protocol. International journal of environmental research and public health 19: 16741.
- Bommarito PA, Martin E, Fry RC (2017) Effects of prenatal exposure to endocrine disruptors and toxic metals on the fetal epigenome. Epigenomics 9: 333-350.
- de Masi S, Bucagu M, Tunçalp Ö, Peña-Rosas JP, Lawrie T, et al. (2017) Integrated Person-Centered Health Care for All Women During Pregnancy: Implementing World Health Organization Recommendations on Antenatal Care for a Positive Pregnancy Experience. Global health, science and practice 5:197-201.
- Mate A, Reyes-Goya C, Santana-Garrido Á, Vázquez CM (2021) Lifestyle, Maternal Nutrition and Healthy Pregnancy. Current vascular pharmacology 19: 132-140.
- Szyf M (2021) Perinatal stress and epigenetics. Handb Clin Neurol 180: 125-148.
- Montagnoli C, Zanconato G, Cinelli G (2020) Maternal mental health and reproductive outcomes: a scoping review of the current literature. Arch Gynecol Obstet. 302: 801-819.
- Blackmore R, Boyle JA, Gray KM, Willey S, Highet N, et al. (2022) Introducing and integrating perinatal mental health screening: Development of an equity-informed evidence-based approach. Health expectations: an international journal of public participation in health care and health policy 25: 2287-2298.
- Surveillance report 2017 – Antenatal and postnatal mental health: clinical management and service guidance (2014) NICE guideline CG192. (2017) National Institute for Health and Care Excellence (NICE).
- Marshall NE, Abrams B, Barbour LA, Catalano P, Christian P, et al. (2022) The importance of nutrition in pregnancy and lactation: lifelong consequences. American journal of obstetrics and gynecology 226: 607-632.
- Jing YH, Song Y F, Yao YM, Yin J, Wang DG, et al. (2014) Retardation of fetal dendritic development induced by gestational hyperglycemia is associated with brain insulin/IGF-I signals. International journal of developmental neuroscience: the official journal of the International Society for Developmental Neuroscience 37: 15-20.
- Arango C, Dragioti E, Solmi M, Cortese S, Domschke K, et al. (2021) Risk and protective factors for mental disorders beyond genetics: an evidence-based atlas. World psychiatry: official journal of the World Psychiatric Association (WPA) 20: 417-436.
- Rowland J, Wilson CA (2021) The association between gestational diabetes and ASD and ADHD: a systematic review and meta-analysis. Scientific reports 11: 5136.
- Keats EC, Haider BA, Tam E, Bhutta ZA (2019) Multiple-micronutrient supplementation for women during pregnancy. The Cochrane database of systematic reviews 3: CD004905.
- Keats EC, Oh C, Chau T, Khalifa DS, Imdad A, et al. (2021) Effects of vitamin and mineral supplementation during pregnancy on maternal, birth, child health and development outcomes in low- and middle-income countries: A systematic review. Campbell systematic reviews 17: e1127.
- Kinshella M, Omar S, Scherbinsky K, Vidler M, Laura A ,et al. (2021) Effects of Maternal Nutritional Supplements and Dietary Interventions on Placental Complications: An Umbrella Review, Meta-Analysis and Evidence Map. Nutrients Framework Working Group 13: 472.
- Perichart-Perera O, Rodríguez-Cano AM, Gutiérrez-Castrellón P (2020) Relevance of nutritional supplements during pregnancy: Role of iron, folic acid, vitamin D, calcium and multiple micronutrients. Gaceta medica de Mexico 156: S1-S26.
- Poniedzia?ek-Czajkowska E, Mierzy?ski R (2021) Could Vitamin D Be Effective in Prevention of Preeclampsia?. Nutrients 13: 3854.
- Coker SJ, Smith-Díaz CC, Dyson RM, Vissers MCM, Berry MJ (2022) The Epigenetic Role of Vitamin C in Neurodevelopment. International journal of molecular sciences 23: 1208.
- Jacob CM, Newell ML, Hanson M (2019) Narrative review of reviews of preconception interventions to prevent an increased risk of obesity and non-communicable diseases in children. Obesity reviews: an official journal of the International Association for the Study of Obesity 1: 5-17.
- Son JS, Chae SA, Zhao L, Wang H, de Avila JM, et al. (2022) Maternal exercise intergenerationally drives muscle-based thermogenesis via activation of apelin-AMPK signaling. EBioMedicine 76: 103842.
- Wang L, Zhu L (2022) Exercise during pregnancy may have more benefits than we thought. EBioMedicine 77: 103889.
- Popova S, Dozet D, Shield K, Rehm J, Burd L (2021) Alcohol's Impact on the Fetus. Nutrients 13: 3452.
- Sher J (2020) Fetal alcohol spectrum disorders: preventing collateral damage from COVID-19. The Lancet. Public health 5: e424.
- Abraham M, Alramadhan S, Iniguez C, Duijts L, Jaddoe, VW, et al. (2017) A systematic review of maternal smoking during pregnancy and fetal measurements with meta-analysis. PloS one 12: e0170946.
- Pinheiro EA, Stika CS (2020) Drugs in pregnancy: Pharmacologic and physiologic changes that affect clinical care. Seminars in perinatology 44: 151221.
- Grenier LN, Atkinson SA, Mottola M F, Wahoush O, Thabane L, et al. (2021) Be Healthy in Pregnancy: Exploring factors that impact pregnant women's nutrition and exercise behaviours. Maternal & child nutrition 17: e13068.
- Avram M J (2020) Pharmacokinetic studies in pregnancy. Seminars in perinatology 44: 151227.
- Joseph P, Vettraino IM (2020) Cannabis in Pregnancy and Lactation - A Review. Missouri medicine 117: 400-405.
- Al-Haddad BJS, Oler E, Armistead B, Elsayed NA, Weinberger DR, et al. (2019) The fetal origins of mental illness. American journal of obstetrics and gynecology 221: 549-562.
- Atif N, Lovell K, Rahman A (2015) Maternal mental health: The missing "m" in the global maternal and child health agenda. Semin Perinatol 39: 345-352.
- Alderdice F, McNeill J, Lynn F (2013) A systematic review of systematic reviews of interventions to improve maternal mental health and well-being. Midwifery 29: 389-399.
- Fernández Y Fernández-Arroyo M, Muñoz I, Torres J (2014) Assessment of the pregnancy education programme with 'EDUMA2' questionnaire in Madrid (Spain). J of Eval in clin pract 20: 436-444.
- Taylor RM, Wolfson JA, Lavelle F, Dean M, Frawley J, et al. (2021) Impact of preconception, pregnancy, and postpartum culinary nutrition education interventions: a systematic review. Nutri reviews 79: 1186-1203.
- Tsakiridis I, Oikonomidou AC, Bakaloudi DR, Dagklis T, Papazisis G, ,et al (2021) Substance Use During Pregnancy: A Comparative Review of Major Guidelines. Obstet Gynecol Survey 76: 634-643.
- McIntosh JE, Olsson CA, Schuijers M, Tan ES, Painter F, et al. (2021) Exploring Perinatal Indicators of Infant Social-Emotional Development: A Review of the Replicated Evidence. Clin Child Fam Psychol Rev 24: 450-483.
- Family Health Service (2020) Antenatal and Postnatal Mental Health. Department of Health. The Government of the Hong Kong Special Administrative Region.
- Rogers A, Obst S, Teague SJ, Rossen L, Spry EA, et al. (2020) Association Between Maternal Perinatal Depression and Anxiety and Child and Adolescent Development: A Meta-analysis. JAMA pediatrics 174: 1082-1092.
- Srinivasan R, Pearson RM, Johnson S, Lewis G, Lewis G (2020) Maternal perinatal depressive symptoms and offspring psychotic experiences at 18 years of age: a longitudinal study. The lancet. Psychiatry 7: 431-440.
- Vacheron MN, Dugravier R, Tessier V, Deneux-Tharaux C (2022) Suicide maternel périnatal: comment prévenir ? [Perinatal maternal suicide: How to prevent?]. L'Encephale 48: 590-592.
- Trost SL, Beauregard JL, Smoots AN, Ko JY, Haight SC, et al. (2021) Preventing Pregnancy-Related Mental Health Deaths: Insights From 14 US Maternal Mortality Review Committees, 2008-17. Health affairs (Project Hope) 40: 1551-1559.
- Jahanfar S, Howard LM, Medley N (2014) Interventions for preventing or reducing domestic violence against pregnant The Cochrane database of systematic reviews 11: CD009414.
- Mazza M, Caroppo E, Marano G, Chieffo D, Moccia L, et al. (2021) Caring for Mothers: A Narrative Review on Interpersonal Violence and Peripartum Mental Health. Int J of Environ Res and Pub Health 18: 5281.
- De Vito M, Alameddine S, Capannolo G, Mappa I, Gualtieri P, et al. (2022) Systematic Review and Critical Evaluation of Quality of Clinical Practice Guidelines on Nutrition in Pregnancy. Healthcare (Basel, Switzerland) 10: 2490.
- Fernández Fernández-Arroyo M(2020) Childbirth Education: Comparative Analysis. IntechOpen.
- Jardim DMB, Modena CM (2018) Obstetric violence in the daily routine of care and its characteristics. Revista latino-americana de enfermagem 26: e3069.
Citation: Fernández, Matilde (2023) Interventions for Mental Health Care in Gestation and Puerperium Review. J Reprod Med Gynecol Obstet 8: 154.
Copyright: © 2023 Matilde Fernández y Fernández-Arroyo, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

