Nutrition and Physical Exercise for the Prevention and Management of Diabetes
*Corresponding Author(s):
Ashok ChakrabortySacred Heart University, Connecticut, United States
Tel:+1 2036409433,
Email:chakrabortya@sacredheart.edu
Abstract
Diabetes is the disease that occurs when hyperglycemia develops. Hyperglycemia is when blood sugar becomes far higher than normal (70 and 99 mg/dL). Generally, when fasting blood glucose level becomes equal to or greater than 126 mg/dL it is considered diabetic. The symptoms for this disease are increased thirst, fatigue, irritability, frequent urination, and the presence of ketones in urine to just name a few. There are two types of diabetes and both have different causes. Type-1 diabetes is caused when body’s immune system attacks and destroys insulin making beta cells of pancreas, and therefore, reducing the availability of insulin. Type-2 diabetes is caused by genetic abnormality or may be some unknown reason that creates insulin resistance.
Some examples of food that can help maintain proper blood glucose levels are discussed here along with the importance of physical exercise to control diabetes. If diets and lifestyle changes are taken seriously, diabetes can be managed or even avoided.
Keywords
Diabetes Type-1 and Type-2; Insulin; Nutrition; Physical exercise; Prevention and management
INTRODUCTION
Diabetes
Diabetes is actually a case of hyperglycemia, which means a rise in blood glucose level beyond the normal value (70 and 99 mg/dL). This disease is very common across the globe and its prevalence continues to increase every year [1]. The prevalence of this disease in USA is estimated to increase from 425 million people in 2017 to 629 million by 2045, with linked health, social, and economic costs [1,2]. Epidemiological studies revealed that diabetes is mostly caused due to lack of proper eating habits [3]. However the level of sugar (glucose) in the blood is very critical; below or higher of its level could be detrimental to human health. Low glucose levels cause hypoglycemia, while an excess can cause diabetes. A fasting blood glucose level equal to or greater than 126 mg/dL is considered diabetic.
During the normal process of digestion, food is consumed and broken down into small sugar particles called glucose. The glucose enters the blood stream and is moved into the body’s cells, where it can be used as energy. Diabetes is a chronic disease in which food is not properly absorbed in the body to be used as energy, and the results in high levels of sugar in the blood.
Cause of diabetes
Normally the glucose level in the body is controlled by two enzymes that come from the Pancreas, one is glucagon which increases the blood glucose level when it is lower than normal; and the second is insulin which decreases the glucose level from blood by transporting them to the cells for energy production (ATP) (Figure 1). Therefore, when the insulin supply from the Pancreas becomes low or none, blood glucose level increases and diabetes develops. The first type of diabetes (Type-1) develops when auto-immune death of pancreas cells occurs, while in the other type (Type-2) insulin resistance develops. The causes of diabetes may include genetic defects, virus, and more commonly inappropriate food habits and sedentary life style [3-7]. Type-1 diabetes develops when there is an auto-immune death of pancreas cells, whereas, Type-2 diabetes occurs when the body develops a resistance to insulin.
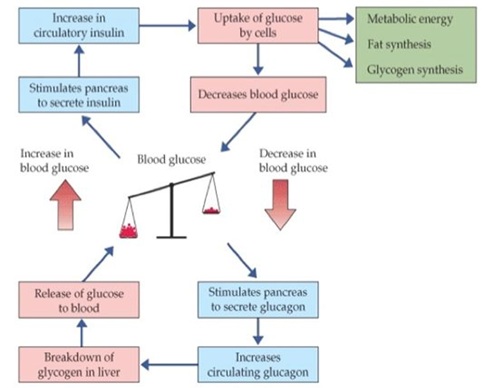 Figure 1: Hormones and control of blood glucose.
Figure 1: Hormones and control of blood glucose.
Symptoms of diabetes
The disease increases thirst, excessive hunger, fatigue, blurred vision, weight loss or gain. Over time, kidney failure and heart disease may appear [8].
Prognosis of diabetes
Over time, diabetes can damage the heart, blood vessels, eyes, kidneys, and nerves. Adults with diabetes have a two- to three-fold increased risk of heart attacks and strokes [9]. Combined with reduced blood flow, neuropathy (nerve damage) in the feet increases the chance of foot ulcers, infection and eventual need for limb amputation. Diabetic retinopathy is an important cause of blindness, and occurs as a result of long-term accumulated damage to the small blood vessels in the retina. 2.6% of global blindness can be attributed to diabetes [10]. Diabetes is among the leading causes of kidney failure [11].
Present treatment options for diabetes
The treatments for diabetes vary from insulin therapy, to diets, to exercise. The risk of heart diseases (high blood pressure and damages blood vessels) is four times higher in diabetic people than people without diabetes [12]. Therefore, in addition to medication (insulin administration), exercise, and weight control and regulated diets can help manage the symptoms of diabetes better.
Other options for prevention and better management of diabetes
A question that arises from this is what else besides medicinal help, such as insulin administration, can be done Nutrition and Physical exercise to better manage diabetes.
Nutrition and diabetes
Nutrition is a key factor for prevention of diabetes and helping to maintain blood glucose levels in the blood with healthier diets. Along with, weight management is a cornerstone of metabolic health and thus physical exercise. Evidence supports that avoiding processed foods, refined grains, processed red meats, and sugar sweetened drinks, but increasing to consume fiber, vegetables, and yoghurt, are beneficial to prevent diabetes, strokes, heart disease, kidney failure, avoidance of blurred vision and influence of weight loss or gain [13-15]. In a meta-analysis of a Randomized Controlled Trial (RCT) with interventions >4 weeks among people with diabetes, participants on a low-GI diet (GI, glycemic Index) had a significant reduction in HbA1C than those on a high-GI diet [16].
What food are recommended and not recommended for Diabetes
Mono and polyunsaturated fats (e.g., olive oil, canola oil, nuts/seeds, avocado), fatty fish (particularly those are high in omega-3 fatty acids e.g., salmon, herring, trout, Sardines, fresh tuna), skinless poultry, nonfat or low-fat dairy, and legumes while considered good to consume; sugary beverages, trans fats, dried fruits are not recommended for diabetic people [17]. Beef, pork, lamb and high-fat dairy products (e.g., cream cheese, whole milk or yogurt), as they contain high saturated fat and may be associated with increased cardiovascular risk are also not recommended either.
How food components work
Soluble fiber interventions have been shown to reduce HbA1C and plasma fasting glucose in people with diabetes [18]. Overconsumption of high fructose-sweetened beverages has adverse effects on selective deposition of visceral fat, lipid metabolism, blood pressure, insulin sensitivity, and de novo lipogenesis in overweight and obese individuals [19]. However, naturally occurring fructose from whole fruits is unlikely to be deleterious because of its relatively slow digestion and absorption unless consumed in an excess amount (>10% of energy) [20]. Nonnutritive sweeteners may have potential to reduce overall calorie and carbohydrate intake [21].
Proteins
There is no such report on restriction of protein consumption for Diabetic people [20]. Rather, it is important to maintain or increase protein intake for people on energy-reduced diets for weight-loss because using a fixed percentage of total calories to estimate a protein requirement may result in inadequate protein intake and lean muscle loss [20].
Fats
Evidence indicates that the type of fat consumed is more important than total fat intake in supporting metabolic goals [22]. In a cohort study of women with diabetes, greater intake of saturated fat and cholesterol was associated with higher CVD risk [23], and greater intake of fish and long-chain omega-3 PUFA from food was associated with lower coronary heart disease incidence [24].
Dietary patterns
Several dietary patterns consisting of combinations of different foods or food groups are beneficial for diabetes management. The DASH (Dietary Approaches to Stop Hypertension) diet has been shown to lower blood pressure among people without (or controlled) diabetes [25,26]. However, in an experiment with a small 8-week RCT among people with diabetes, the DASH diet, including the 2,400mg/d sodium restriction, had favorable effects on glycemic control, high-density lipoprotein and Low-Density Lipoprotein (LDL) cholesterol, blood pressure, and inflammatory biomarkers [27,28].
Several low-fat vegetarian or vegan diet trials in people with diabetes did not show any improvement on glycemic control or CVD risk was reported [29].
Vitamin and mineral supplementation
The current nutrition therapy recommendations do not support vitamin or mineral supplementation in people with diabetes who do not have underlying deficiencies [20,21,30]. However, people with diabetes should consider the importance of acquiring daily vitamin and mineral requirements through a well-balanced diet, as they often experience micronutrient deficiencies, especially the elderly, pregnant and lactating women, vegetarians, and those are on calorie-restricted diets, but have diabetes [21].
Physical exercise and diabetes
The current nutritional therapy recommendations from various organizations for diabetes management support intensive lifestyle interventions to achieve modest weight-loss and weight-maintenance [20,21,30,31]. Physical exercise maintains healthy body weight and reduces the risk of diabetes, along with other benefits like; it strengthens heart, immune system [32]. Both aerobic and resistance training programs promote healthier skeletal muscle, adipose tissue, liver, and pancreatic function, whole-body insulin sensitivity [33-35].
PE and nutrition works together to manage diabetes
Aerobic exercise is useful for increasing the body’s use of oxygen and stimulating cardiovascular health, while stretching and resistance training are good for cardio-respiratory and musculoskeletal fitness, as well as improves flexibility and body composition [36]. Therefore, it appears that nutrition and physical activity as they depend on each other, goes simultaneously and works synergistically (Figure 2). Many diseases are instigated by poor diet and lack of exercise.
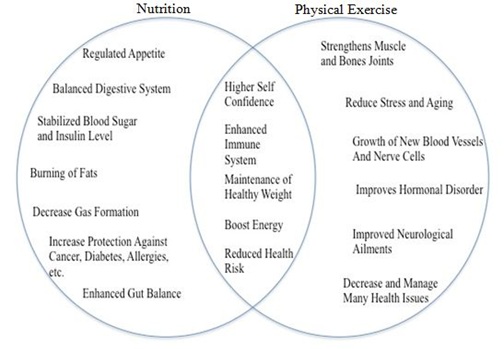 Figure 2: Benefits of nutrition and physical exercise when goes together.
Figure 2: Benefits of nutrition and physical exercise when goes together.
Nutrition and Physical exercise are two necessities of life that can go hand in hand in many situations. Without both, people can experience growth stunts or even delays in certain vital processes including physical as well mental development. Exercise definitely is important for maintaining physical health, but it is deeply reliant on nutrition for maintaining a healthy body and mind (emotional and physical health). Moreover, exercise cannot be done efficiently if proper nutrition is not maintained.
Aerobic or resistance exercise
Which one is better: Aerobic exercise consists of continuous, rhythmic movement of large muscle groups, such as in walking, jogging, and cycling. It is notably well-established that aerobic exercise can improve Hb1Ac, insulin sensitivity, oxidative capacity, and important related metabolic parameters [37].
Resistance training
During the last 2 decades, resistance training has gained considerable recognition as a viable exercise training option for patients with type-2 diabetes. Synonymous with strength training, resistance exercise involves movements utilizing free weights, weight machines, body weight exercises, or elastic resistance bands. Primary outcomes in studies evaluating the effects of resistance training in type-2 diabetes have found improvements that range from 10% to 15% in strength, bone mineral density, blood pressure, lipid profiles, cardiovascular health, insulin sensitivity, and muscle mass [33,38].
Combining aerobic and resistance training
Cuff et al., 24 evaluated whether a combined training program could improve insulin sensitivity beyond that of aerobic exercise alone in 28 postmenopausal women with type-2 diabetes. Indeed, 16 weeks of combined training led to significantly increased insulin-mediated glucose uptake compared with a group performing only aerobic exercise, reflecting greater insulin sensitivity [39]. Balducci et al., demonstrated that combined aerobic and resistance training markedly improved HbA1c compared with the control group and globally improved risk factors for cardiovascular disease [39]. Since the supporting evidences are in favor of combined training, American Diabetes Association (ADA) recommended a guideline for the combination of aerobic and resistance training, combination modalities for controlling glucose and lipids in type-2 diabetes.
SUMMARY AND GLOBAL PERSPECTIVES
In the past two decades, evidence from prospective cohort studies has surged to highlight the importance of individual nutrients, foods, and dietary patterns in type-2 diabetes prevention and management. The convergence of dietary factors for prevention and management of diabetes was observed, and healthful dietary patterns for diabetes prevention and management were typically rich in whole grains, fruits and vegetables, nuts, legumes, moderate in alcohol consumption, and lower in refined grains, red/processed meats. To achieve long-term adherence, individuals can have flexibility in food choices without compromising overall diet quality.
The vast majority of present knowledge on dietary prevention and management of diabetes have been derived from Western populations. It is critically important to conduct original investigations in other populations with different disease susceptibility and eating habits. Evidence-based nutrition therapy recommendations have been developed and implemented in many developed countries [20,21,30]. However, further development of region specific guidelines is needed to provide practical educational instruments considering variation in dietary patterns, accessibility to food, and agriculture in different regions and cultures.
Global efforts, such as homogenizing standardization of front-of-package nutrition labels and nutrition facts in conjunction with public education campaigns, will reshape the nutritional transition and the global food supply helping to curb the type-2 diabetes epidemics.
CONCLUSION
This article reviews how proper nutrition and physical exercise together are required for the prevention and better management of Diabetes, and indicates what can increase insulin sensitivity. Exercising 5 hours per week, especially the resistance training; to build lots of muscle mass and consuming higher intakes of vegetables; whole-grain foods, legumes, lean proteins, and nuts/seeds; supplements like omega-3 fatty acids, alpha-lipoic acid, and chromium; adequate vitamin D; and limiting caffeine intake should be the goal.
Nutrition is often said to be the cornerstone of diabetes care. The goal for nutritional management is optimal metabolic control through a balance between food intakes, physical activity. In type-2 diabetes, proper nutrition can improve glycemic and lipid levels and help weight loss when required. In type-1 diabetes, the goal of nutritional intervention can improve glycemic control through coordination of food, especially carbohydrates, doses of insulin, and physical activity.
A diabetic’s life is very different from a normal, non-diabetic life, living with many difficult symptoms every day. There are many foods that are recommended for diabetic people to control their blood sugar levels. There are, however, also a large number of foods that are restricted and should be minimized in a diabetic’s nutrition. This article provides some guidelines, like recommended diets and also regular physical activity, to achieve a healthy life, free from diabetes.
ACKNOWLEDGEMENT
We acknowledge our colleagues and support staff members for editorial help, especially to Ms. Amrita Guha, (Senior, Boston University), also for providing information during the writing this article.
REFERENCES
- Syed Amin Tabish (2007) Is Diabetes Becoming the Biggest Epidemic of the Twenty-first Century? Int J Health Sci 1: V-VIII.
- International Diabetes Federation (2017) IDF diabetes atlas.8th ed. IDF, Brussels, Belgium.
- Sami W, Ansari T, Butt NS, Hamid MRA (2017) Effect of diet on type 2 diabetes mellitus: A review. Int J Health Sci (Qassim) 11: 65-71.
- Baker PR, Steck AK (2011) The past, present, and future of genetic associations in type 1 diabetes. Curr Diab Rep 11: 445-453.
- Andersen MK, Pedersen CE, Moltke I, Hansen T, Albrechtsen A, et al. (2016) Genetics of Type 2 Diabetes: the Power of Isolated Populations. Curr Diab Rep 16: 65-73.
- Chatterjee S, Khunti K, Davies MJ (2017) Type 2 diabetes. Lancet 389: 2239-2251.
- Christopher MF and Matthias H (2008) Viral Trigger for Type 1 Diabetes. Diabetes 57: 2863-2871.
- https://www.niddk.nih.gov/health-information/diabetes/overview/symptoms-causes
- Emerging Risk Factors Collaboration, Sarwar N, Gao P, Seshasai SR, Gobin R, et al. (2010) Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet 26: 375: 2215-2222.
- Bourne RR, Stevens GA, White RA, Smith JL, Flaxman SR, et al. (2013) Causes of vision loss worldwide, 1990-2010: a systematic analysis. Lancet Glob Health 1: 339-349.
- Saran R, Li Y, Robinson B, Ayanian J, Balkrishnan R, et al. (2015) US Renal Data System 2014 Annual Data Report: Epidemiology of Kidney Disease in the United States. Am J Kidney Dis 66: 1-305.
- Healthline (2018) Type 2 Diabetes and High Blood Pressure: What’s the Connection? Healthline, New York, USA.
- Mohammad A (2014) The prevention and control the type-2 diabetes by changing lifestyle and dietary pattern. J Educ Health Promot 3: 1-12.
- Gray A, Threlkeld RJ (2019) Nutritional Recommendations for Individuals with Diabetes. In: Feingold KR, Anawalt B, Boyce A, et al. (eds). Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc, Massachusetts, Bristol.
- Nordström K, Coff C, Jönsson H, Nordenfelt L, Görman U (2013) Food and health: individual, cultural, or scientific matters? Genes Nutr 8: 357-363.
- Thomas DE, Elliott EJ (2010) The use of low-glycaemic index diets in diabetes control. Br J Nutr 104: 797-802.
- Nowak C, Weinhouse B (2019) 38 Fat-Burning Foods to Help You Lose Weight. The Healthy, New York, USA.
- Silva FM, Kramer CK, de Almeida JC, Steemburgo T, Gross JL, et al. (2013) Fiber intake and glycemic control in patients with type 2 diabetes mellitus: a systematic review with meta-analysis of randomized controlled trials. Nutr Rev 71: 790-801.
- Stanhope KL, Schwarz JM, Keim NL, Griffen SC, Bremer AA, et al. (2009) Consuming fructose-sweetened, not glucose-sweetened, beverages increases visceral adiposity and lipids and decreases insulin sensitivity in overweight/obese humans. J Clin Invest 119: 1322-1334.
- Canadian Diabetes Assocaition Clinical Practice Guidelines Expert Committee (2013) Clinical Practice Guidelines: Nutrition Therapy. Can J Diabetes 37: 45-55.
- Evert AB, Boucher JL, Cypress M, Dunbar SA, Franz MJ, et al. (2014) Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care 37: 120-143.
- Estruch R, Ros E, Salas-Salvadó J, Covas MI, Corella D, et al. (2013) Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med 368: 1279-1290.
- Tanasescu M, Cho E, Manson JE, Hu FB (2004) Dietary fat and cholesterol and the risk of cardiovascular disease among women with type 2 diabetes. Am J Clin Nutr 79: 999-1005.
- Hu FB, Cho E, Rexrode KM, Albert CM, Manson JE (2003) Fish and long-chain omega-3 fatty acid intake and risk of coronary heart disease and total mortality in diabetic women. Circulation 107: 1852-1857.
- Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, et al. (1997) A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med 336: 1117-1124.
- Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, et al. (2001) Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med 344: 3-10.
- Azadbakht L, Fard NRP, Karimi M, Baghaei MH, Surkan PJ, et al. (2011) Effects of the Dietary Approaches to Stop Hypertension (DASH) eating plan on cardiovascular risks among type 2 diabetic patients: a randomized crossover clinical trial. Diabetes Care 34: 55-57.
- Azadbakht L, Surkan PJ, Esmaillzadeh A, Willett WC (2011) The Dietary Approaches to Stop Hypertension eating plan affects C-reactive protein, coagulation abnormalities, and hepatic function tests among type 2 diabetic patients. J Nutr 141: 1083-1088.
- Ajala O, English P, Pinkney J (2013) Systematic review and meta-analysis of different dietary approaches to the management of type 2 diabetes. Am J Clin Nutr 97: 505-516.
- Mann JI, De Leeuw I, Hermansen K, Karamanos B, Karlström B, et al. (2004) Evidence-based nutritional approaches to the treatment and prevention of diabetes mellitus. Nutr Metab Cardiovasc Dis 14: 373-394.
- Dyson PA, Kelly T, Deakin T, Duncan A, Frost G, et al. (2011) Diabetes UK evidence-based nutrition guidelines for the prevention and management of diabetes. Diabet Med 28: 1282-1288.
- https://medlineplus.gov/benefitsofexercise.html
- Colberg SR, Sigal RJ, Yardley JE, Riddell MC, Dunstan DW, et al. (2016) Physical Activity/Exercise and Diabetes: A Position Statement of the American Diabetes Association. Diabetes Care 39: 2065-2079.
- Kirwan JP, Solomon TPJ, Wojta DM, Staten MA, Holloszy JO (2009) Effects of 7 days of exercise training on insulin sensitivity and responsiveness in type 2 diabetes mellitus. Am J Physiol Endocrinol Metab 297: 151-156.
- Magkos F, Tsekouras Y, Kavouras SA, Mittendorfer B, Sidossis LS (2008) Improved insulin sensitivity after a single bout of exercise is curvilinearly related to exercise energy expenditure. Clin Sci (Lond) 114: 59-64.
- Luan X, Tian X, Zhang H, Huang R, Li N, et al. (2019) Exercise as a prescription for patients with various diseases. Journal of Sport and Health Science 8: 422-441.
- Zanuso S, Jimenez A, Pugliese G, Corigliano G, Balducci S (2010) Exercise for the management of type 2 diabetes: a review of the evidence. Acta Diabetol 47: 15-22.
- Gordon BA, Benson AC, Bird SR, Fraser SF (2009) Resistance training improves metabolic health in type 2 diabetes: a systematic review. Diabetes Res Clin Pract 83: 157-175.
- Balducci S, Leonetti F, Di Mario U, Fallucca F (2004) Is a long-term aerobic plus resistance training program feasible for and effective on metabolic profiles in type 2 diabetic patients? Diabetes Care 27: 841-842.
Citation: Guha S, Chakraborty A, Arnold N, Belotti L, Boudreault B, et al. (2020) Nutrition and Physical Exercise for the Prevention and Management of Diabetes. J Cell Biol Cell Metab 7: 018.
Copyright: © 2020 Smita Guha, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.