
Perinatal Testicular Torsion - Clinical and Ultrasound Findings of a Rare Pathology
*Corresponding Author(s):
Maria São PedroDepartment Of Pediatrics, Centro Hospitalar Barreiro-Montijo, Barreiro, Portugal
Tel:+351 212147300,
Email:mia.sps@gmail.com
Abstract
Perinatal Testicular Torsion (PTT) is a very rare event, occurring before or at birth in 70% cases and the remaining, within the first month of life. Most PTT are extravaginal, thus being a separate clinical entity from testicular torsions seen later in life. Clinical presentation and ultrasonographic signs varies accordingly to the time elapsed since the torsion. Apart from clinical examination, Doppler ultrasonography constitutes the ground for diagnosis.
We present two male newborns with unilateral scrotal changes noted in the first day of life. The first had an elevated, horizontally displaced, hard and enlarged left testicle. An enlarged right scrotum with a non-tender mass was found in the second case. Neither had irritability nor signs of pain. Doppler ultrasonography showed, in both cases, unilateral testicular enlargement with abnormal echo structure and absence of blood flow, consistent with PTT.
Currently, the standard of care seems to be unilateral orchiectomy (if the testis is not salvageable) with contralateral orchiopexy to prevent the devastating effects of anorchia, should asynchronous torsion occur. This was the procedure performed in both cases.
Keywords
Neonatal scrotum; Perinatal testicular torsion; Testicular torsion
INTRODUCTION
Perinatal Testicular Torsion (PTT) is a very rare event [1-3], with estimated incidence of 6:100.000 [2,4,5]. The actual frequency is probably higher as reports of “vanishing testis” are likely from resorption of infarcted testis after an insult [4]. PTT occurs before/at birth (prenatal) or within the first month of life (neonatal) [1,2,5-7]. In approximately 72-81% cases the torsion develops prenatally [7], mostly between the 34th and 36th week of gestation or during labour [1,3,4]. Earlier cases, around the 20th week of pregnancy, have been reported (shown in autopsies of medical abortions) [3].
Most PTT are extravaginal, occurring due to poor adhesion of the tunica vaginalis to the gubernaculum [1,2,4-6], which allows the testis and tunica vaginalis to rotate together around the axis of the spermatic cord, compromising blood flow and leading to ischemia, infarction and necrosis of the testis [1,4-6]. The gubernaculum testis develops during the first 3 months of life, making extravaginal torsion rare beyond this age [1]. The intravaginal torsion, mostly seen later in life in prepubertal boys, has a different pathophysiology in which the testis is not fixed in the tunica vaginalis and can twist freely on its’ pedicle like a bell clapper [2,6,7].
There have been multiple theories regarding why PTT occurs [5,6]. It has been postulated that hypermobility of the tunica vaginalis within the scrotal sac when exposed to an extreme cremasteric reflex, during delivery or in utero, may induce a torsion [5]. Intrauterine stress may be a significant risk, such as prolonged or difficult/traumatic labor, high birth weight, twin gestation, breech presentation, preeclampsia, gestational diabetes or vaginal delivery [1,5-7]. In addition, there may be a role for genetic factors, as this entity has been also reported in siblings [6].
Differential diagnosis with pathological lesions of the neonates’ scrotum should be made, including scrotal hematoma, orchiepididymitis, hydrocele, inguinal hernia, testicular tumors and meconial periorchitis [1,2,7].
CASE REPORT
Two full-term male newborns, appropriate for gestational age, presented unilateral scrotal changes in the first day of life. The first one, born from vaginal delivery and the second one from c-section due to fetal distress, both with apgar scores 9 and 10 at 1 and 5 minute, respectively. Pregnancies were uneventful, highlighting only maternal essential arterial hypertension, controlled with methyldopa, in the second newborn’s case. Mothers were caucasian, aged 27 and 31 years old.
In the first case, an elevated, horizontally displaced, hard and enlarged left testicle was noticed (Figure 1(a)). An enlarged right scrotum with a non-tender mass was found in the second case (Figure 1(b)). In both cases, a bluish color of the ipsilateral scrotum and a contralateral hydrocele was seen (Figure 1). Neither had irritability nor signs of pain.
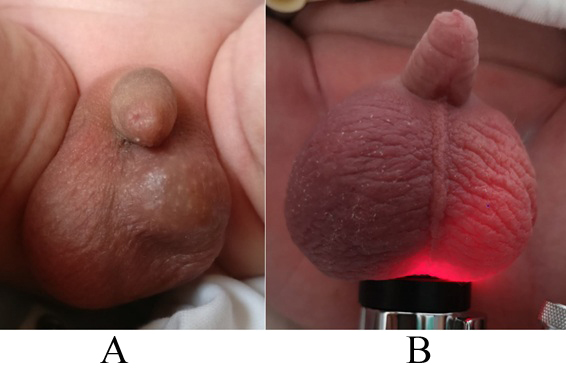 Figure 1: Clinical presentation at the time of surgery ((a) First newborn, (b) Second newborn, with transillumination test).
Figure 1: Clinical presentation at the time of surgery ((a) First newborn, (b) Second newborn, with transillumination test).
Urgent Doppler ultrasonography was performed and showed, in both cases, unilateral testicular enlargement with abnormal echo structure and absence of blood flow, consistent with PTT (Figure 2). In the first case a marked heterogeneous echo texture with hypo/anechoic central areas and peripheral “eggshell-like” calcification (tunica albuginea calcification), suggestive of old necrosis, was found (Figure 2(a)). An altered “reniform” testicular morphology with non-homogeneous echoes and radial hypoechoic areas (suggestive of testicular lobular edema), associated with a diffuse increased echogenicity of tunica albuginea and subtunical fluid, was evident in the second case (Figure 2(b)). In both cases a contralateral hydrocele (and ipsilateral in the second case) was apparent.
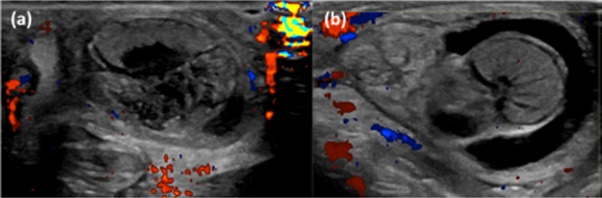 Figure 2: High-frequency color Doppler ultrasound examination findings ((a) First newborn; (b) Second newborn).
Figure 2: High-frequency color Doppler ultrasound examination findings ((a) First newborn; (b) Second newborn).
In both cases, an urgent unilateral orchiectomy with contralateral orchidopexy was performed.
DISCUSSION
In most cases, PTT develops prenatally, and the testicle undergoes irreversible necrosis [2]. It had been previously reported that PTT occurred more frequently on the left side, possibly owing to differences in the testicular vasculature [5]. However, recent studies have shown no predilection on side [1,5]. Bilateral forms, both synchronous and asynchronous, were described in 10% of cases [1,3,5,6].
Clinical presentation is different in prenatal and neonatal torsion [1,2,4,7]. If prenatal, depending on its timing, the clinical examination can vary from: no palpable testicle; a small atrophic hard mass; an enlarged livid color scrotum with an indurated unpainful mass [1,2,4]. Neonatal torsion has a similar clinical presentation to testicular torsions seen later in life, with acute swelling and redness of the scrotum [1,2]. In both types of PTT, pain/irritability are not characteristic nor needed for diagnosis and must not delay it [2].
Regarding its clinical findings, our cases were consistent with a prenatal event. The first one probably occurred earlier because of its harder consistency with no enlargement of the scrotum. The blueish coloration seen in either case, is due to the hemorrhagic extravasation secondary to the venous occlusion [1]. Assessing for cremasteric reflex is not very relevant, since only 48% of healthy children have it at birth [1].
Apart from clinical examination, ultrasound evaluation (Mode B and Doppler) is the gold-standard for diagnosis [1,2,4], being frequently considered conclusive [2].
Ultrasound findings closely correlates with the time elapsed since the torsion. It is important to assess not only testicular perfusion but also its size and morphology since it varies with time [1,7]. In the acute phase, the testis and epididymis became enlarged with an external echogenic ring due to tunica albuginea’s edema [1,4], as seen in our second case. As ischemia progresses, testicular parenchyma gets non-homogeneous [1,7] and radial hypoechoic areas, suggestive of testicular lobular edema [1], might be seen, as also manifested in the second case. The continuous absence of blood flow to the testis leads to a hypoxic-ischemic injury making the testis progressively heterogenic with hypo/anechoic central areas, which corresponds to infarction and necrosis histologically [1,2,4,7]. This pattern was found in the first case, in which central and peripheral “eggshell-like” calcification could also be seen. Calcification appears in torsions with weeks of evolution, increasing with time, thus being suggestive of old necrosis [1,7]. This support our previous conjecture of the first case being an “oldest” torsion. With time, the testis became small and atrophic with a hyperechoic ring due to tunica albuginea’s calcification [1,2,4].
An ipsilateral hydrocele, resulting from changes in vascularization or inflammation [1], which is present in the second case, might be the first sign of a perinatal testicular torsion, even before changes in testicle size and structure manifests [1,7]. A contralateral hydrocele is also present in up to 60% cases [1,4], as seen in both our cases and may be the consequence of secondary inflammatory reaction after contralateral torsion or congenital abnormality due to incomplete closure of the processus vaginalis [3]. It may also reflect the general incidence in neonatal population with no correlation with the torsion [3].
The absence of blood flow within the testicular parenchyma in Doppler evaluation is also an important sign [1-4,7], having high specificity for the diagnosis of PTT [7]. However, it should be underlined that, even for healthy newborn boys, the evaluation of blood flow in testis might be difficult, because of its natural lower flow state [2,4]. In such cases high-frequency color Doppler ultrasound should be used to increase sensitivity [4,7]. Nonetheless, at a torsion’s early stage the testicular vein is still patent, therefore, the presence of testicular blood flow does not rule out PTT [7].
Owing to PTT rarity, its management is controversial [1,2,5,6]. Even with an early diagnosis, salvage rates have been reported at about 5%, thus the need for urgent intervention has been heavily debated [5,6].
On the other hand, bilateral PTT requires emergent treatment, because of its high possibility of anorchia [1]. Neonatal PTT also requires emergent surgical intervention, making its salvage rate go up to 21% [1,2]. Testicle ischemia leads to irreversible changes: spermatogenesis is lost within 4-6 hours; and Leydig cells, responsible for testosterone production, undergo destruction after 12 hours.
Regarding prenatal torsions, there are two positions, both based on salvaging rates and possibility of synchronous or asynchronous contralateral torsion. The existence of described cases of contralateral torsion between 8 hours to 6 months after the first torsion, supports early contralateral orchidopexy [1,5]. The detractors of this early exploration defend the low percentage of testicles that are saved and the surgical risk involved [1].
Regardless of its timing, orchiectomy is often recommended to prevent damage of the contralateral germinal epithelium (triggered by cytokines [1] or possibly by antibodies [2,5]) and because of risk of infection and malignant degeneration, described in up to 10% of cases [1-3,5].
Recent studies suggest that exploration of the contralateral testis in a unilateral PTT is mandatory, in order to evaluate the testis’ real condition and fix it, thus preventing a future contralateral torsion and anorchia [5,6].
CONCLUSION
PTT is a rare entity, different from testicular torsions seen later in life. The authors highlight the importance of clinical scrotum exam, since pain and irritability are non-specific symptoms. Our cases show a continuum of clinical and ultrasound findings that can be seen in prenatal PTT. Although testicular viability was probably already compromised, particularly in the first case, an urgent approach was warranted for the possibility of current or future asynchronous torsion, thus preventing anorchia and its catastrophic consequences.
REFERENCES
- Nebot CS, Salvador RL, Aliaga SP, Iñigo EG (2017) Torsión testicular perinatal. Valoración ecográfica y diagnóstico diferencial. Radiología 59: 391-400.
- Przemys?aw B, Warcho? S, Brzewski M, Majkowska Z, Warcho? TD, et al. (2016) Ultrasonography of extravaginal testicular torsion in neonates. Pol J Radiol 81: 469-472.
- Sauvestre F, André G, Harran MH, Hemard M, Carles D, et al. (2016) Prenatal testicular torsion: Not always in the late third trimester. Urology 89: 132-133.
- Ganni P, Vachhani N, Udayasankar U (2014) Intrauterine testicular torsion. J Urol 191: 217-218.
- Monteilh C, Calixte R, Burjonrappa S (2018) Controversies in the management of neonatal testicular torsion: A meta-analysis, J Pediatr Surg 54: 815-819.
- Pakmanesh H, Alinejad M (2018) A case of bilateral perinatal testicular torsion that presented with unilateral torsion; necessity of contralateral testis exploration. Turk J Urol 44: 511-514.
- Xiao H, Gao Y, Li Y, Tang Y, Zhu L, et al. (2016) Ultrasound assessment of perinatal testicular torsion. Br J Radiol 89: 20151077.
Citation: São Pedro M, Vale G, Simões M, Albuquerque J, Lacerda C, et al. (2020) Perinatal Testicular Torsion - Clinical and Ultrasound Findings of a Rare Pathology. J Neonatol Clin Pediatr 7: 055.
Copyright: © 2020 Maria São Pedro, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

