
Platelet Rich Plasma in the Treatment of Frontal Fibrosing Alopecia
*Corresponding Author(s):
Thais P PincelliDepartment Of Dermatology, Mayo Clinic, 4500 San Pablo Rd, Jacksonville, FL 32224, United States
Tel:+1 9049536402,
Fax:+1 9049532590
Email:Pincelli.Thais@mayo.edu
Abstract
Frontal Fibrosing Alopecia (FFA) represents a form of scaring alopecia more frequent in postmenopausal women that presents with frontal hairline recession. It is typically classified as a variant of lichen planopilaris. Treatment of FFA can be challenging with poor long-term outcomes.
Platelet-Rich Plasma (PRP) consists of an autologous concentration of platelets in a small volume of plasma. Activated platelets secrete cytokines and growth factors and thus may have a potential role in the treatment of inflammatory scarring alopecia such as FFA.
A 68-year-old female with multi-resistant FFA was treated with lesional PRP injections every 4 weeks for 16 weeks. Baseline LPPAI score and phototrichograms targeting a representative area of disease activity were compared at baseline and at 16 weeks.
After 16 weeks, no significant change in follicular units or follicular density from baseline to week 16 was noted. Only a minimal improvement in inflammatory activity observed clinically and through the Lichen Planopilaris Activity Index was observed. The discordance between the follicular density count and observed inflammatory activity suggests a longer treatment and observational period is needed. Additionally, the frequency of PRP injections potentially may also need to be increased.
Given the limited efficacy of current therapies for FFA, PRP injections may be an option in patients with refractory disease, as an adjunct to systemic therapy. Additional investigation is needed to optimize frequency of PRP injections in FFA and to better assess its true anti-inflammatory effect.
Case Presentation
Frontal Fibrosing Alopecia (FFA), a lymphocytic mediated scaring alopecia, predominates in postmenopausal women and presents with frontal hairline recession and frequent eyebrow and eyelash involvement [1-3]. While typically classified as a variant of lichen planopilaris, the pathogenetic relationship with FFA remains unexplained along with the factors leading to the dramaticallyincreased worldwide prevalence over the last decade [4,5]. Treatment of FFA is challenging with highly variable responses and poor long-term outcomes [3,6].
Platelet-Rich Plasma (PRP) is a type of regenerative therapy consisting of an autologous concentration of platelets in a small volume of plasma [7]. Because activated platelets secrete numerous cytokines and growth factors, PRP may promote hair growth in the declining hair follicle. Recently, PRP has also been shown to stimulate dermal papillae cell proliferation, thereby increasing survival of hair follicle cells and thus may have a potential role in the treatment of inflammatory scarring alopecia such as FFA.
A 68-year-old female with FFA who previously failed treatment with interlesional Kenalog, finasteride, and hydroxychloroquine was treated with lesional PRP injections given every 4 weeks for 16 weeks. 60 mL of blood were collected from a peripheral vein and 3 mL of PRP was prepared according to the standardized Mayo Clinic Regenerative PRP preparation protocol and was injected to affected areaof the scalp using a 30-gauge needle. Injections were well tolerated, and no adverse events were noted. Baseline LPPAI score and phototrichogramstargeting a representative area of disease activity were compared at baseline and at 16 weeks.
There are several challenges in evaluating the efficacy of therapies for FFA. First, patients must be early enough in their disease course to achieve a meaningful clinical effect as scarring alopecia results in irreversible follicular destruction. Second, the onset of FFA is often very gradual and may be characterized bylow-grade inflammatory activity that is often difficult to appreciate clinically and only becomes noticeable after significant hair loss.The patient in this pilot was selected for not only failing standard therapy but also because the inflammatory activity of her condition was readily assessable (Figures 1a&1b) and the duration of disease was less than three years.
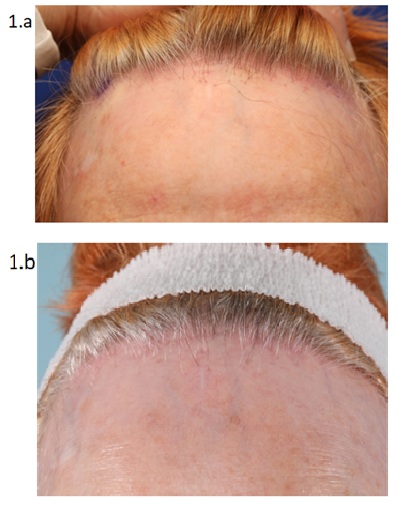 Figure 1a&1b: Clinical photographs (1a & 1b): There was only a minimal improvement in the degree of inflammatory activity
Figure 1a&1b: Clinical photographs (1a & 1b): There was only a minimal improvement in the degree of inflammatory activity
After 16 weeks, no significant change in follicular units or follicular density from baseline to week 16 was noted (Figure 2). However, there also was only a minimal improvement in the degree of inflammatory activity observed clinically or scored through the Lichen Planopilaris Activity Index (Figure 1b). These findings have implications for the study design of future trials evaluating the efficacy of PRP for FFA, as resolution of inflammation generally correlates with the arrest offollicular destruction. The discordance between the follicular density count and observed inflammatory activity suggests a longer treatment and observational period is needed. Additionally, the frequency of PRP injections potentially may also need to be increased asonly mildanti-inflammatory effects were observed with monthly injections after 16 weeks. 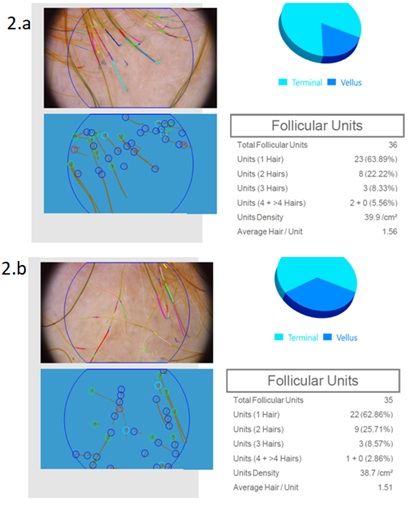
Figure 2: Phototrichograms (2a & 2b) at baseline and at 16 weeks, after 4 sessions of PRP injections, 1 month apart. After 16 weeks, no significant change in follicular units or follicular density from baseline to week 16 was noted
Conclusion
Given the limited efficacy of current therapies for FFA, treatment with PRP injections may be an option in patients with refractory disease possibly as an adjunct to oral therapy as they appear well tolerated. However, further investigation through clinical trials is needed to optimize frequency of PRP injections in FFA and to better assess the true anti-inflammatory potential of PRP overall.
References
- Tavakolpour S, Mahmoudi H, Abedini R, Hesari KK, Kiani A, et al. (2019) Frontal fibrosing alopecia: An update on the hypothesis of pathogenesis and treatment. Int J Womens Dermatol 5: 116-123.
- Bolduc C, Sperling LC, Shapiro J (2016) Primary cicatricial alopecia: Lymphocytic primary cicatricial alopecias, including chronic cutaneous lupus erythematosus, lichen planopilaris, frontal fibrosing alopecia, and Graham-Little syndrome. J Am Acad Dermatol 75: 1081-1099.
- Vano-Galvan S, Molina-Ruiz AM, Serrano-Falcón C, Arias-Santiago S, Rodrigues-Barata AR, et al. (2014) Frontal fibrosing alopecia: a multicenter review of 355 patients. J Am Acad Dermatol 70: 670-678.
- Imhof RL, Chaudhry HM, Larkin SC, Torgerson RR, Tolkachjov SN (2018) Frontal Fibrosing Alopecia in Women: The Mayo Clinic Experience With 148 Patients, 1992-2016. Mayo Clin Proc 93: 1581-1588.
- MacDonald A, Clark C, Holmes S (2012) Frontal fibrosing alopecia: a review of 60 cases. J Am Acad Dermatol 67: 955-961.
- Mardones F, Shapiro J (2017) Lichen planopilaris in a Latin American (Chilean) population: demographics, clinical profile and treatment experience. Clin Exp Dermatol 42: 755-759.
- Lubkowska A, Dolegowska B, Banfi G (2012) Growth factor content in PRP and their applicability in medicine. J Biol Regul Homeost Agents 26: 3-22.
Citation: Pincelli TP, Arthurs JR, Sluzevich JC (2021) Platelet Rich Plasma in the Treatment of Frontal Fibrosing Alopecia. J Clin Dermatol Ther 7: 091.
Copyright: © 2021 Thais P Pincelli, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

