The Myocardial Perfusion Scintigraphy: A New Noninvasive Exploration of Children Cardiac Pathologies in Benin
*Corresponding Author(s):
Badiane SMDepartment Of Biophysics, Nuclear Medicine, UFR Of Health Sciences, Gaston BERGER University Of Saint-Louis, Senegal
Email:drmoussabadiane@gmail.com
Abstract
Pediatric nuclear cardiology is in progress in the world. Myocardial perfusion scintigraphy has been performing in children since four decades in advanced countries. It is a noninvasive diagnostic tool in the management of pediatric coronary lesions in connection with congenital heart disease or other cardiovascular pathologies. It is performed after injection of technetium radiopharmaceuticals at rest or under physical or pharmacological stress. Synchronized with the ECG, it allows the evaluation of myocardial kinetics, end-systolic and end-diastolic volumes of the left ventricle and the systolic ejection fraction. It is rarely practiced or almost nonexistent in French-speaking sub-Saharan Africa, in particular in Benin. It will be made available from 2021 at Cotonou in the Mother and Child's Teaching Hospital “Lagune” (CHU-MEL). This awareness article is a summary of the practice of myocardial perfusion scintigraphy in children based on data from the literature.
Keywords
Benin; Child; Myocardial perfusion scintigraphy
INTRODUCTION
Nuclear cardiology was thrived in recent decades with the advent of new scintigraphic image acquisition devices and new radiopharmaceuticals [1,2]. Myocardial perfusion scintigraphy is widely performed in adults in several countries, the main indication being the screening and monitoring of coronary artery disease (exertional myocardial ischemia and myocardial infarction) [3]. The practice of myocardial scintigraphy in children remains limited and little known to practitioners in charge of children. Its indications differ from those of adults and its realization requires specific measures. Unlike developed countries where scintigraphy is common practice, several countries in sub-Saharan Africa are struggling to set up scintigraphic imaging centers [4,5]. Benin plans to make available in 2021 the nuclear medicine department at the Mother and Child's Teaching Hospital “Lagune” (CHU-MEL). As a prelude to the implementation of this imaging technic in Benin, we describe in this popularization article the principle, the indications, the technical procedure and the results of myocardial perfusion scintigraphy in children based on the data from the literature. This is also a work to sensitize Beninese doctors to this technique, which enriches the algorithms of pediatric cardiology management.
Principle of performing myocardial scintigraphy
Scintigraphy is a functional imaging technique that studies the distribution of a radiopharmaceutical with an affinity for a given target organ. Myocardial perfusion scintigraphy allows evaluation of relative myocardial perfusion through intravenous administration of a radiopharmaceutical. It makes it possible to detect the territories with a relative defect of fixation and therefore of myocardial perfusion (myocardial ischemia and myocardial infarction). This evaluation of the relative myocardial perfusion can be carried out at rest or after a provocation test for myocardial ischemia (pharmacological stress or stress test) and planar or most often tomographic acquisitions are made. During tomographic acquisitions synchronized with an electrocardiographic signal, synchronized single-photon emission tomography, it is possible to simultaneously evaluate the perfusion and the segmental and global kinetics of the left ventricle [6].
Indications for myocardial perfusion scintigraphy in children
The indications for myocardial perfusion include all pathological situations that may alter coronary arterial flow. The main indications are dominated by the search for myocardial ischemia in the study of congenital heart disease [7-8]. Mention may particularly be made of inflammatory damage to the coronary arteries such as Kawasaki syndrome which manifests itself among other things by vasculitis, sometimes involving coronary arteries, in children under 5 years old, including children and newborns [9]. The evolution towards the constitution of a stenosing fibrosis of the coronary artery at the origin of an ischemia which can be complicated by angina pectoris or myocardial infarction, acute heart failure and rhythm disturbances.
In congenital heart disease, such as tetralogy of Fallot, inter atrial, atrioventricular, inter ventricular communications or aorto-pulmonary fistula, the study of the perfusion of the myocardial walls is indicated during the initial diagnosis and follow-up with conservative treatment or after a heart transplant. In addition to perfusion, myocardial scintigraphy, when synchronized with electrocardiography, makes it possible to study segmental and global kinetics and to estimate the ejection fraction of the left ventricle [6]. This approach may be useful for estimating heart function in children on cardiotoxic chemotherapy and dilated cardiomyopathies. Studies have shown the value of myocardial scintigraphy in children with sickle cell disease [10].
METHODS OF PERFORMING MYOCARDIAL PERFUSION SCINTIGRAPHY IN CHILDREN
Stress and rest exam
Scintigraphy can be done under stress and at rest [6]. The stress examination makes it possible to assess myocardial reserve and to highlight early-stage coronary damage, particularly reversible myocardial ischemia at rest. Physical stress should be preferred as long as it is feasible. It consists of recording the heart's adaptation to effort by measuring heart rate, blood pressure and ECG recording during standardized physical exercise, usually on a treadmill or on a cycloergometer. It is rare that this method can be applied before the age of 6 and it takes 8 to 10 years to achieve smooth collaboration. When the opposite is the case, pharmacological stress is carried out using dipyridamole (0.56 mg / kg in 4 minutes) or adenosine (140 µg / Kg / min over 6 minutes) [7,11,12].
Radiopharmaceuticals
There are two groups of radiopharmaceuticals: technetium tracers and thallium 201. The most widely used technetium tracers are lipophilic cations such as tetrofosmin and Methoxy-isobutyl-isonitril (MIBI), labeled with radioisotope, metastable technetium 99 (99mTc) which decays to stable technetium with a physical half-life of six hours by emitting gamma rays of 140 keV. The activity to be injected is correlated with the mass of the child and varies from 3.7 to 11 MegaBecquerels / Kilograms (MBq / Kg) for each examination (stress and rest). Thallium 201 is an analogue of potassium. It is more irradiating than technetium tracers because of its physical characteristics and not recommended for children. The radiopharmaceuticals used bind to the myocardial walls according to the regional coronary arterial flow at the time of intravenous bolus injection, and remain relatively stable during the acquisition of images [6].
Image acquisition
Image acquisition is carried out by means of a gamma camera, most often in tomographic mode, using the pediatric acquisition protocol. The acquisition starts 15 to 30 minutes after the injection of the technetium tracers and ends less than 20 minutes. Strict immobility of the child is required for a good quality examination. When necessary, physical restraint is performed or sometimes premedication. The synchronization of the tomoscintigraphic images with the electrocardiography makes it possible to study the segmental and global kinetics of the left ventricle and to estimate the systolic ejection fraction. It also improves exam performance [6,13].
Dosimetry
The effective dose depends on the activity administered and it should be in the order of 20 µSv / MBq, or 0.07 to 0.2 mSv per kilogram per examination [6]. This dose is similar to many other irradiating imaging techniques in children.
MYOCARDIAL PERFUSION SCINTIGRAPHY RESULTS IN CHILDREN
Myocardial perfusion analysis
The normal appearance of myocardial perfusion is homogeneous fixation of the radiotracer throughout the myocardium (Figure 1) [7]. In the event of a perfusion abnormality, hypofixation of the radiotracer is observed in the arterial territory involved (Figure 2) [12]. Hypofixation of the radiotracer on stress examination which improves at rest is in favor of myocardial ischemia while a persistence of this hypofixation at rest is characteristic of myocardial necrosis.
Annexes
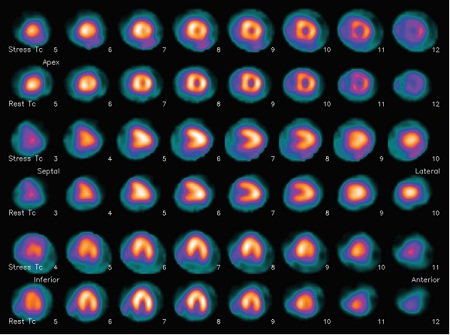 Figure 1: Myocardial perfusion scintigraphy with 99mTc-MIBI of normal appearance under pharmacological stress (adenosine) and at rest in a 4-year-old boy [7].
Figure 1: Myocardial perfusion scintigraphy with 99mTc-MIBI of normal appearance under pharmacological stress (adenosine) and at rest in a 4-year-old boy [7].
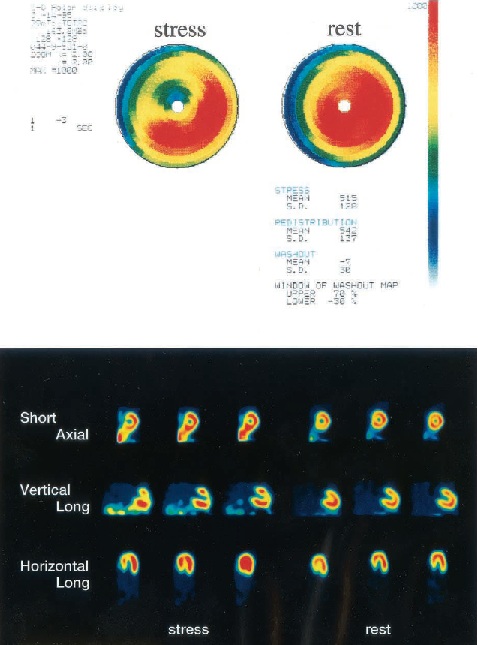 Figure 2: Myocardial perfusion scintigraphy with 99mTc-tetrofosmin at pharmacological stress (dipyridamole) and at rest showing ischemia in a 23-month-old boy followed for Kawasaki disease [12].
Figure 2: Myocardial perfusion scintigraphy with 99mTc-tetrofosmin at pharmacological stress (dipyridamole) and at rest showing ischemia in a 23-month-old boy followed for Kawasaki disease [12].
Analysis of non-perfusion parameters
The synchronization of the tomographic images with the ECG makes it possible to study the kinetics of the myocardial walls, to estimate the end-systolic and end-diastolic volumes of the left ventricle and to deduce its systolic ejection fraction. The study of kinetics makes it possible to decide on cases of questionable interpretation and to improve examination performance [13].
Artifacts and sources of error
The main artefacts and sources of error are related to poor preparation of the radiopharmaceutical, poor image quality, image recording errors, attachment of the radiotracer, an adjacent structure to the heart and movement of the heart during the acquisition. These artifacts and sources of error are mostly preventable if the correct examination protocol is followed [6].
DISCUSSION
Perfusion scintigraphy has been performed in pediatric purpose since several decades in developed countries [14,15]. Indeed, the integrity of the perfusion of the heart by the coronary arteries is obviously vital for the myocardium and it is necessary to evaluate it in some malformative situations or in some acquired pathologies. Coronary angiography is the gold standard in coronary artery disease, highlighting anatomical lesions, but is an invasive and complex technique in children. Myocardial perfusion scintigraphy is non-invasive and low irradiation which assesses the relative coronary flow [6]. It is feasible from the neonatal period for the rest examination, and requires the use of pharmacological stress for the stress examination. Physical effort is achievable in children from 6 years old.
In 2013, in China, Reddy et al [7] had performed myocardial perfusion scintigraphy with 99mTc-MIBI in ten children aged between 1.25 and 6 years old who had been operated on for transposition of the great vessels in order to detect early post complications, acute or chronic operations. Adenosine, used for pharmacological stress, at a rate of 140 μg / kg / min as a continuous intravenous infusion over 6 min, was well tolerated by all children. In Japan in 2007, Takasugi et al [16] had demonstrated the value of myocardial perfusion scintigraphy in the follow-up of children after implantation of a pacemaker for congenital complete atrioventricular block. They had demonstrated a correlation between the defect of myocardial perfusion on scintigraphy and the occurrence of dilated cardiomyopathy. In the 1980s, before the advent of technetium tracers, thallium 201 was the only one radiopharmaceutical for performing myocardial perfusion scintigraphy. Thus, Bjorkhem et al [14] in Sweden reported their experience of myocardial scintigraphy performed with thallium 201 from 1983 to 1989 in 52 children aged 4 days to 18 years. The exam was performed at rest and during physical exertion for some children. The clinical indications concerned coronary artery malformations, Kawasaki syndrome, postoperative monitoring of certain cardiovascular malformations (transposition of large vessels, pulmonary atresia) and dilated or hypertrophic cardiomyopathy. Similarly, Fukazawa et al [17], in Japan in 1993 compared the results of thallium 201 scintigraphy (rest and pharmacological stress with dipyridamole) and coronary angiography for screening for myocardial ischemia in a population of 34 children of 03 to 18 years of age followed for Kawasaki syndrome. They had observed a similarity between scintigraphy and coronary angiography with a sensitivity of the scintigraphy evaluated at 71%. However, they found 25% of cases of discrepancy between the scintigraphy and the coronary angiography with false negatives. The discrepancies between myocardial perfusion scintigraphy and coronary angiography could be related to damage to the microcirculation and the development of collateral circulation network not objectified by coronary angiography [15]. Two years later, in 1995, in Italy, a study carried out by Schillaci et al [18] on a population of 15 children aged 1 to 6 years with Kawasaki syndrome, concluded that the scintigraphy performed better myocardial perfusion in the detection of coronary damage with a sensitivity of 88% and a specificity of 93%. The same observation was made during a study carried out in 2002 in Japan by Fukuda et al [12] who had used tetrofosmin labeled with 99mTc as a radiotracer to perform scintigraphy and dipyridamole for pharmacological stress on a sample of 86 children between the ages of 3 and 10 years with Kawasaki syndrome. The examination was well tolerated by the children, and the performance of the examination in detecting significant coronary lesions was close to coronary angiography with 90% sensitivity and 100% specificity.
The synchronization of myocardial perfusion with electrocardiography in children was tested in 2011, in Turkey by Hallioglu et al [10], to assess the value of the practice of myocardial perfusion scintigraphy of 99mTc-MIBI synchronized with the ECG on a population of 43 sickle cell children aged 6 to 18 years. They were able to objectify that more than a third of the children had a dilation of the left ventricle measured by the synchronized scintigraphy with the ECG. In addition, they had established a good correlation between synchronized scintigraphy and echocardiography. The measurement of the volume of the left ventricle by myocardial scintigraphy is an important parameter to take into account in the monitoring and evaluation of children with sickle cell disease, they concluded. Recently, in 2016, Sugiyama et al [8], in Japan, compared the performance of myocardial perfusion scintigraphy on a population of 107 newborns aged 2 to 30 days operated for transposition of the great vessels. The scintigraphy was performed with tetrofosmin labeled with 99mTc metastable at rest and then coupled with pharmacological stress with dipyridamole. They had observed that there was a correlation between the results of the scintigraphy and those of the coronary angiography. In fact, the depth of the hypofixation of the radiotracer was proportional to the anatomical lesions demonstrated on the coronary angiography. They concluded that the combination of the two examinations would allow better postoperative follow-up and an evaluation of the prognosis in children operated on for transposition of the great vessels.
While several authors were interested in myocardial perfusion scintigraphy in the study of the left ventricle, a Canadian team, led by Velasco-Sanchez [19], had shown in 2012 the feasibility of perfusion of the right ventricle with myocardial scintigraphy with 99mTc-MIBI at rest and under physical stress in a sample of healthy children of mean age 11.1 ± 3.3 years. His team had further established a relationship between the level of fixation of the right ventricle and that of the left ventricle that could be exploited in the assessment of congenital and acquired heart disease in the child. In sub-Saharan Africa, pediatric nuclear cardiology is still rudimentary. Indeed, Adambounou et al [20], had analyzed the repertoire of pediatric scintigraphic examinations carried out from 2009 to 2017 in Senegal, one of the few countries in the sub-region with a nuclear medicine service. Of the 40 or so scintigraphy examinations performed in children, there was no myocardial perfusion scintigraphy. This reflects the difficulty of access to the examination in the country or the little interest given by practitioners in studying myocardial perfusion in heart disease in children by scintigraphy.
CONCLUSION
Myocardial perfusion scintigraphy has been performed in developed countries for more than four decades. It is a non-invasive, low-radiation diagnostic tool that correlates well with coronary angiography in the assessment of coronary heart disease in children. This functional imaging modality will be available in Benin at the Mother and Child's Teaching Hospital “Lagune” in 2021. This will contribute to better management of pediatric coronary damage. Efforts must be made by the authorities and health actors to promote it in French-speaking sub-Saharan Africa.
REFERENCES
- van Dijk JD, Jager PL, van Dalen JA (2019) The next step in standardizing SPECT myocardial perfusion imaging. West Afr J radio 15: 22-27
- Songy B (2010) Nouvelles caméras cardiaques à semi-conducteur cadmium–zinc–telluride (CZT) et scintigraphies myocardiques au thallium 201. Médecine Nucléaire 34: 473-479.
- Jau P, Jacob T, Lecorff G, Bouvier JL, Novella P, et al. (2010) Place de la scintigraphie myocardique dans l’angor stable. Médecine Nucléaire 34: 178-183.
- Obioha FI (2008) Nuclear medicine practice in Africa. West Afr J Radio 15: 22-27.
- Tahirou I, Moussa IDJ, Ada A, Djeomboro I, Moustapha A, et al. (2012) Analyse des résultats préliminaires de scintigraphie myocardique réalisée à l’institut des radio-isotopes (IRI) du Niger. À propos de 37 cas. Médecine Nucléaire 36: 591-599.
- Djaballah W, Manrique A, Marie PY, Rouzet F, Songy B, et al. (2012) Guide pour la rédaction de protocoles pour la tomoscintigraphie de perfusion myocardique. Médecine Nucléaire 36: 336-352.
- Reddy A, Bisoi AK, Singla S, Patel CD, Das S (2013) Adenosine stress myocardial perfusion scintigraphy in pediatric patients after arterial switch operation. Indian journal of nuclear medicine 28: 210-215.
- Sugiyama H, Tsuda E, Ohuchi H, Yamada O, Shiraishi I (2016) Chronological changes in stenosis of translocated coronary arteries on angiography after the arterial switch operation in children with transposition of the great arteries: comparison of myocardial scintigraphy and angiographic findings. Cardiol Young 26: 638.
- Bajolle F (2012) La maladie de Kawasaki. EMC – Angéiologie 7: 1-10.
- Hallioglu O, Gunay EC, Unal S, Erdogan A, Balci S, et al. (2011) Gated Myocardial Perfusion Scintigraphy in Children with Sickle Cell Anemia: Correlation with Echocardiography. Rev Esp Med Nucl 30: 354-359.
- Manrique A, Marie PY, Maunoury Ch, Acar Ph, Agostini D (2002) Mise à jour des recommandations concernant la pratique des épreuves de provocation d'ischémie en cardiologie nucléaire chez l'adulte et l'enfant. Médecine Nucléaire 26: 691-709.
- Fukuda T, Ishibashi M, Yokoyama T, Otaki M, Shinohara T, et al. (2002) Myocardial ischemia in Kawasaki disease: evaluation with dipyridamole stress technetium 99m tetrofosmin scintigraphy. Journal of nuclear cardiology 9: 632-637.
- Dunet V, Costo S, Sabatier R, Grollier G, Bouvard G, et al. (2010) Faisabilité et précision diagnostique d’un protocole de scintigraphie myocardique synchronisée à l’ECG en deux heures: l’étude Myofast. Médecine Nucléaire 34: 211-218.
- Björkhem G, Evander E, White T, Lundström NR (1990) Myocardial scintigraphy with 201 thallium in pediatric cardiology: a review of 52 cases. Pediatric cardiology 11: 1-7.
- Ueda K, Saito A, Nakano H, Yano M (1980) Thallium 201 scintigraphy in an infant with myocardial infarction following mucocutaneous lymph node syndrome. Pediatric radiology 9: 183-185.
- Takasugi H, Watanabe K, Ono Y, Sakaguchi H, Motoki N, et al. (2008) Myocardial scintigraphy after pacemaker implantation for congenital complete atrioventricular block. European journal of pediatrics, 167: 183-188.
- Fukazawa M, Fukushige J, Takeuchi T, Narabayashi H, Igarashi H, et al. (1993) Discordance between thallium-201 scintigraphy and coronary angiography in patients with Kawasaki disease: myocardial ischemia with normal coronary angiogram. Pediatric cardiology 14: 67-74.
- Schillaci O, Banci M, Scopinaro F, Tavolaro R, Villotti G, et al. (1995) Myocardial scintigraphy with 99mTc-sestamibi in children with Kawasaki disease. Angiology 46: 1009-1014.
- Velasco-Sanchez D, Lambert R, Turpin S, Laforge S, Fournier A, et al. (2012) Right ventricle myocardial perfusion scintigraphy: feasibility and expected values in children. Pediatric cardiology 33: 295-301.
- Adambounou K, Bathily EAL, Djigo S, Mbodj M, Ndoye O (2017) Pediatric Nuclear Medicine Examinations Realized In Senegal from 2009 to 2017: General Characteristics and Diagnostic Contribution. J Nucl Med Radiat Ther 8: 5.
Citation: Hounkponou M, Houndetoungan GD, Fachinan OH, Badiane SM, Amoussou-Guenou KM (2020) The Myocardial Perfusion Scintigraphy: A New Noninvasive Exploration of Cardiac Pathologies Child in Benin. J Nucl Med Radiol Radiat Ther 5: 027
Copyright: © 2020 Hounkponou M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.