Visual Cues for Persons with Dementia: Opinions of Dementia Caregivers & Occupational Therapists
*Corresponding Author(s):
Linda StruckmeyerDepartment Of Occupational Therapy, University Of Florida, 1225 Center Drive, Gainesville, Florida, 32610, United States
Email:lstruckmeyer@phhp.ufl.edu
Abstract
Introduction: There are gaps in the literature on the use of visual cues by persons with dementia, especially in regards to which type of visual cues dementia caregivers find to be the most useful for activities of daily living (ADLs) and how occupational therapists view the use of visual cues in the homes of their clients with dementia.
Methods: The study included a focus group of dementia caregivers (n=7) and a survey of occupational therapists (n=8). The primary aim of the focus group was to identify the opinions of dementia caregivers on the usefulness of the different types of visual cues for ADLs in the home environment. The secondary aim was to identify which type of visual cue caregivers deem to be the most useful type for completing ADLs. The survey aimed to gather occupational therapists’ professional opinions on: 1) the usefulness of visual cues for both the safety and participation of persons with dementia, 2) caregiver implementation of visual cues, and 3) reasons for client inability to use visual cues.
Results: Three major themes emerged from the focus group: organizational cues are more useful for caregivers than care recipients, written cues are less helpful for more advanced stages of dementia, and environmental cues are the most helpful overall. The results of the survey indicate that visual cues improve safety and participation. The therapists were in agreement with the caregivers on environmental cues being the most helpful type of visual cue. The results of the survey also imply that cognition dysfunction is the main reason for client inability to use visual cues. The results of the focus group support this finding.
Discussion: Visual cues are an important domain to consider in the evaluation of persons with dementia in their home.
Keywords
Dementia; Visual cues; Activities of daily living; Safety; Participation; Aging in place
Introduction
Dementia is an age-related disorder that is associated with a decline in cognition and independence [1]. Alzheimer’s disease is the most common type of dementia. Over 5 million Americans currently have Alzheimer’s disease, and this number is projected to rise to almost 14 million by the year 2050 [2]. Maintaining independence in activities of daily living (ADLs) has been associated with a greater health-related quality of life in persons with dementia [1]. Thus, as more persons with dementia are electing to age in place, home modifications are becoming more pertinent. One home modification that can facilitate aging in place is visual cues, as they can be used to facilitate ADLs and to improve safety and participation in persons with dementia [3]. There are three different types of visual cues: environmental cues, written cues, and organizational cues [4].
Environmental cues include color-coding and the placement of items in view for task completion. Several studies suggest that they are an effective intervention for persons with dementia. For instance, Soilemezi et al. identified that dementia caregivers value the use of color-coding [5]. Wherton et al. identified that dementia caregivers and care recipients value the placement of medicine bottles and personal hygiene items in view for use [3]. Keller et al. identified that caregivers find several different environmental cues, such the placement of a measuring cup in view, to be useful for promoting cooking [6]. In line with that finding, Gitlin et al. found that an intervention involving the placement of items in view for task completion, such as the task of making a salad, to be effective [7]. Likewise, Nomura et al. found that an intervention that included placing kitchen utensils in view improved the proficiency of persons with dementia in the kitchen [8]. O’Connor et al. also found that placing ingredients in view aided in care recipient participation in cooking [9].
Written cues include labels, notes, signs, and lists. In relation to safety concerns, way signs along with environmental cues, such as unique pieces of art on walls, appear to aid persons with dementia in navigating through the home environment [10-12]. Several studies have also identified that care recipients find whiteboards, notes, and bulletin boards to be useful for carrying out ADLs [4,6,13-16]. As further evidence of the value of written cues, Judge et al. found that an intervention that included the use of labels and lists was useful for persons with dementia [17]. Similarly, Nomura et al. found that an intervention that included the use of ingredient labels and to do lists improved the proficiency of persons with dementia in the kitchen [8]. Taken together, these studies suggest that written cues are an effective intervention for persons with dementia.
Organizational cues include planners, pill organizers, and calendars. Studies have found that dementia caregivers and care recipients value the use of calendars [5,13] Boger et al. identified that dementia caregivers find medicine organizers to be useful for reminding care recipients to take medications [14]. Also, interventions that implemented the use of calendars for either scheduling or as reminders to take medications were found to be useful in several studies [17-20]. Notably, an intervention, which included the use of planners and notebooks, statistically improved ADLs and memory [21]. Taken together, these studies suggest that organizational cues are an effective intervention for persons with dementia.
Study Aims
Although studies have implied that visual cues are an effective intervention, there are several research gaps that this study aimed to address through the use of a focus group of caregivers of persons with dementia and a survey of home health occupational therapists. The primary aim of the focus group was to identify the opinions of caregivers of persons with dementia on the usefulness of the different types of visual cues for ADLs in the home environment. The secondary aim of the focus group was to identify which type of visual cue caregivers deem to be the most useful type for completing ADLs. The survey aimed to gather occupational therapists’ professional opinions on: 1) the usefulness of visual cues for both the safety and participation of persons with dementia, 2) caregiver implementation of visual cues, and 3) reasons for client inability to use visual cues.
Methods
Institutional review board approval was obtained for both the focus group and the survey. All participants consented prior to participation.
Participants
For the focus group, the goal was to have seven to nine participants. The inclusion criteria included that all of the participants must be between the ages of 18 and 89 and serve as a caregiver of a person with dementia who lives at home. The participants were recruited by handing out and posting flyers at a clinic that offers day care services to persons with dementia.
For the survey, the goal was to have 20 participants. The inclusion criteria was that the participants must be registered and licensed occupational therapists practicing in the United States who work with persons with dementia living in the home or home-like environments. Participants were recruited through a secure email by the principal investigator (PI) of the study. They were professional contacts of the PI who had previously indicated interest in this type of study or had previously agreed to be contacted for research.
Data Collection
For the focus group, the demographic data was analyzed using descriptive analysis. The audio recording was transcribed by one member of the research team and reviewed by the other members. Then, the audio recording was destroyed. A thematic coding approach was used. Two members of the research team independently used the transcript to code the data and to identify any possible themes. They then discussed their codes and themes before presenting a finalized version to the PI for review and feedback. The themes were then presented to a qualitative research group for additional feedback. Based on the feedback, two of the proposed major themes were combined into one major theme.
For the survey, the demographic information was categorized. Descriptive statistics were used to analyze the close-ended questions. The answers from the open-ended question were analyzed for content and coded by the research team members independently. The research team members read over each other’s themes and discussed any differences. This information was then presented to a qualitative research group for verification.
Data Analysis
For the focus group, the demographic data was analyzed using descriptive analysis. The audio recording was transcribed by one member of the research team and reviewed by the other members. Then, the audio recording was destroyed. A thematic coding approach was used. Two members of the research team independently used the transcript to code the data and to identify any possible themes. They then discussed their codes and themes before presenting a finalized version to the PI for review and feedback. The themes were then presented to a qualitative research group for additional feedback. Based on the feedback, two of the proposed major themes were combined into one major theme.
For the survey, the demographic information was categorized. Descriptive statistics were used to analyze the close-ended questions. The answers from the open-ended question were analyzed for content and coded by the research team members independently. The research team members read over each other’s themes and discussed any differences. This information was then presented to a qualitative research group for verification.
Results
Focus group
The focus group had seven participants. One participant was a caregiver of a person with mild dementia, two were caregivers of persons with moderate dementia, and four were caregivers of persons with more advanced dementia. Six participants were females, and one was a male.
Major themes
Three major themes, as illustrated by Figure 1, were identified. The themes were 1) organizational cues were more useful for caregivers than for persons with dementia, 2) environmental cues were most useful for persons with dementia, 3) written cues were less useful during the more advanced stages of dementia.
The first theme was that organizational cues were more useful for caregivers than for persons with dementia. Four participants shared that organizational cues are more useful for caregivers than for care recipients. For instance, according to one participant, “The pill container is really for me… Calendars, no forget it, that’s for me.”
The second theme was that environmental cues were most useful for persons with dementia. Six participants had implemented the use of environmental cues in the home environment. Also, when asked which type of visual cues they felt was the most useful, five participants affirmed that environmental cues are the most useful type. Unexpectedly, the participants mentioned placing items out of view, in addition to the placement of items in view. For instance, one participant stated, “I made sure there was nothing toxic on the counter because she would go in and just you know mix all kinds of weird stuff that was inedible.”
The third theme was that written cues were less useful during the more advanced stages of dementia. Four participants discussed written cues being less useful for more advanced stages, due to the language loss associated with dementia. For example, one participant stated, “She’s really at the point to where I really don’t know if she’s understanding any letter or words that she’s reading… In recent times, we’ve had the names of her cats and family members as well, on the dry erase board. But, she’s not really reading those anymore” (Figure 1).
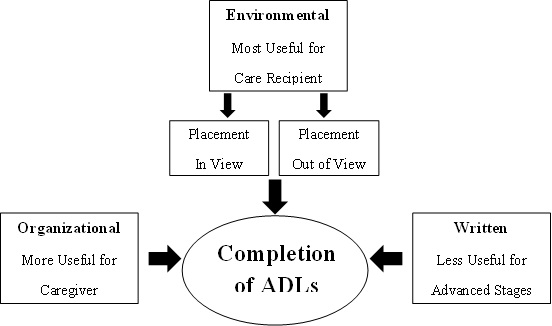 Figure 1: Major themes as related to completion of ADL’s.
Figure 1: Major themes as related to completion of ADL’s.
Secondary themes
Four secondary themes, not directly related to the aims of this study were identified. These were 1) the importance of maintaining a sense of independence, 2) concerns about the person with dementia becoming lost in their home environment, 3) concerns about language loss, and 4) concerns about dressing challenges.
The first secondary theme was about the importance of maintaining a sense of independence. Three participants discussed how their care recipients value maintaining a sense of independence. For example, one participant shared, “She knows where the bathroom is, but I don’t think she wants me to tell her, you know what I’m saying. I think that still, independence is still in there.”
The next secondary theme was concerns about the person with dementia becoming lost in their home environment. Four participants discussed their care recipients becoming lost in the home environment. For example, one participant stated, “Sometimes, she can find the bathroom. Other times, she can’t.”
The third secondary theme was concerns about language loss. Five participants discussed loss of language. For example, one participant shared, “My mother has lost a lot of her language. I mean some of her words, a lot of her words don’t make sense. But she’ll do hand motions.”
The last secondary theme was concerns about dressing challenges. Four participants discussed how challenging the ADL of dressing had become. These challenges included the care recipients not wanting to change into pajamas before bed, not being able to independently dress, and wanting to wear similar outfits each day. For example, one participant stated, “She has like a uniform she wants to wear. I pull out a blue shirt and a pair of jeans, but always the same clothes because she doesn’t want to wear anything else.”
Survey
The survey consisted of 13 questions that included demographic information, four Likert scale questions with a four point scale, two questions about specific types of visual cues, and one open ended question for comments or suggestions related to visual cues. During the six weeks of the survey distribution, 24 contacts were sent emails requesting participation. 14 responses were collected, yet only eight participants met the inclusion criteria. Table 1 summarizes the eight participants’ demographic information. The majority of the participants had been practicing for over 16 years. All but one participant worked with persons with dementia in the home environment. They practiced occupational therapy in four different states (Table 1).
|
Characteristic |
N |
% |
|
State California Connecticut Florida Missouri |
1 1 5 1 |
22.22 11.11 55.56 11.11 |
|
Years Practicing 0-5 6-10 11-15 16+ |
1 0 2 5 |
12.50 0.00 25.00 62.50 |
|
Setting Home Nursing Home |
7 1 |
87.50 12.50 |
Note. N=8.
Table 1: Demographic Information of Survey Participants.
The first Likert-scale question regarded the importance of visual cues for safety of persons with dementia. The second question regarded the importance of visual cues for participation of persons with dementia. The third question regarded the overall benefit of visual cues to clients, while the fourth question regarded the level of caregiver implementation of visual cues. The participants felt that visual cues were important for safety, with half of the participants selecting “important” and the other half selecting “very important”. The participants also felt that visual cues were important for participation, with five participants selecting “important” and three selecting “very important”. A majority of the survey participants also agreed that clients frequently benefit from visual cues. However, in regards to caregiver implementation of visual cues, there was a split in opinion. Five participants selected “rarely” while three selected “frequently”. Table 2 summarizes the responses to the four Likert-Scale survey questions (Table 2).
|
Question |
Response |
% |
Response |
% |
Response |
% |
Response |
% |
|
|
not important |
|
somewhat important |
|
important |
|
very important |
|
|
Importance to safety |
0 |
0.00 |
0 |
0.00 |
4 |
50.00 |
4 |
50.00 |
|
Importance to participation |
0 |
0.00 |
0 |
0.00 |
5 |
62.50 |
3 |
37.50 |
|
|
|
|
|
|
|
|
|
|
|
|
never |
|
rarely |
|
frequently |
|
always |
|
|
Benefit to client |
0 |
0.00 |
0 |
0.00 |
7 |
87.50 |
1 |
12.50 |
|
Caregiver implementation |
0 |
0.00 |
5 |
62.50 |
3 |
37.50 |
0 |
0.00 |
Note. N=8.
Table 2: Frequency of Responses for Likert Scale Questions.
Overall, the most helpful visual cue proved to be environmental cues (item grouping, familiar objects, and color contrast). The most useful environmental cue was found to be item grouping (placement of items in view for task completion), with seven of the participants selecting it. The participants also considered written cues (labels, way signs, and written instructions) to be helpful. The most useful written cue was found to be labels, with six of the participants selecting it. The survey also sought opinions on visual assistive technology. High- and low-tech visual assistive technology were found to be less helpful than the environmental and written cues. As for reasons for client inability to implement visual cues, cognitive dysfunction was the highest recorded reason, with six participants listing it. Table 3 summarizes the specific types of cues that the participants considered to be the most helpful and the reasons the participants provided for client inability to implement the cues (Table 3).
|
Question |
Response |
% |
|
Type of cue |
|
|
|
low-tech visual assistive technology |
2 |
6.06 |
|
contrasting colors |
5 |
15.15 |
|
way signs |
3 |
9.09 |
|
labels |
6 |
18.18 |
|
familiar images |
6 |
18.18 |
|
posted instructions |
4 |
12.12 |
|
item grouping |
7 |
21.21 |
|
Reasons for inability to implement |
|
|
|
impaired vision |
4 |
28.57 |
|
reluctance to use |
2 |
14.29 |
|
cognitive dysfunction |
6 |
42.86 |
|
accessibility of cue |
1 |
7.14 |
|
motor planning “other” |
0 1 |
0.00 7.14 |
Note. N=8.
Table 3: Frequency of Responses for “type of cue” and “inability to implement” Questions.
Four responses were collected for the open-ended question that requested the participants to respond with any other comments or suggestions on the use of visual cues in the home environment. Although the data was limited, three initial recurring themes were found: 1) visual accessibility, 2) placing objects out of sight, and 3) keeping the cues personally relevant to the client.
Discussion
This pilot study was limited in that it only included one focus group of seven participants and one survey of eight participants. Thus, the findings are preliminary and will require further inquiry. However, the results do add to the current knowledge of the efficacy of the use of visual cues in the homes of persons with dementia. Notably, this study was the first to the researcher team’s knowledge to ask dementia caregivers to compare the usefulness of the three types of visual cues for completing ADLs in the home environment. Overall, three major themes and four secondary themes were identified from the focus group. The results indicate that environmental cues are the most helpful visual cue for completing ADLs. The results of the survey indicate that occupational therapists find visual cues to be helpful for both safety and participation in the home environment of persons with dementia, with environment cues being the most helpful.
A strength of the study was that there was consensus between the focus group and the survey results. Both the caregivers and the therapists valued environmental cues and placing dangerous items out of view. Also, the results of the survey suggest that cognitive dysfunction is the main reason that visual cues are misused. The results of the focus group support this idea, as the caregivers viewed written cues to be less beneficial for more advanced stages of dementia. The caregivers also discussed their family members becoming lost in their own homes and experiencing language loss. This finding on cognitive dysfunction is consistent with the current literature, as dementia is a progressive neurological disease. Thus, the stage of dementia should be considered when implementing visual cues.
Additionally, visual impairments were selected by half of the survey participants as a reason for not implementing visual cues. Although none of the focus group participants expressed concerns over visual impairments, this finding is consistent with the literature. According to Armstrong et al., it is important to consider visual impairments when assessing the practicality of visual cues [23]. Nonetheless, visual cues cannot be ignored in regards to persons with dementia who also have visual impairments. Lawrence et al. found that this can lead to further distress and disorientation in both caregivers and care recipients [24]. In addition to impaired vision and cognitive dysfunction, studies have also identified distrust, accessibility, and motor planning as other reasons for not implementing visual cues [10,25-27]. Thus, a client-centered approach to implementing visual cues appears to be the most effective way to improve safety and participation in persons with dementia who elect to age in place.
There was one major area in which the survey and the focus group had conflicting results: caregiver implementation of visual cues. The therapists had a remarkable split in opinion on this area. While three therapists felt that caregivers frequently implement the use of visual cues, the other five therapists felt that caregivers rarely implement the use of visual cues. In contrast, the caregivers of the focus group had all utilized visual cues. The methods of the study could account for this. The participants of the focus group were given background information on visual cues, as well as provided examples of the different visual cues. Yet, the therapists were expected to be familiar with visual cues and thus were not given any background information.
Conclusion
This study examined the opinions of caregivers of persons with dementia on the usefulness of visual cues for completing ADLs and the opinions of occupational therapists on the use of visual cues in the homes of their clients with dementia. Overall, the findings of this study were supported by the current literature and contribute to the current knowledge of the benefits of using visual cues in the homes of persons with dementia. The findings of this study also suggest several areas for future research. One such area is addressing caregiver implementation of visual cues, as the survey and the focus group had conflicting results. Another area is clarifying whether the usefulness of each type of visual cue is dependent upon the stage of dementia. Research on auditory and tactile cues has indicated that the usefulness of these cues is dependent on the stage of dementia [26]. Based on the results of the focus group, it seems likely that the types of visual cues will follow a similar pattern. Overall, further research on visual cues will benefit the growing population of persons with dementia choosing to age in place by enhancing safety and participation in ADLs.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Acknowledgments
The authors would like to thank everyone who participated in the focus group and the survey, as well as the members of the qualitative research group. Margaret Bird, research assistant, is acknowledged for her assistance in editing this manuscript.
References
- Chan CS, Slaughter SE, Jones CA, Wagg AS (2015) Greater independence in activities of daily living is associated with higher health-related quality of life scores in nursing home residents with dementia. Healthcare 3: 503-518.
- Alzheimer's Association (2020) 2020 Alzheimer's disease facts and figures. Alzheimer's Dementia 16: 391-460.
- Wherton JP, Monk AF (2008) Technological opportunities for supporting people with dementia who are living at home. International Journal of Human-Computer Studies 66: 571-586.
- Bourgeois MS (2007) Memory books and other graphic cuing systems: Practical communication and memory aids for adults with dementia. Baltimore: Health Professions Press.
- Soilemezi D, Kallitsis P, Drahota A, Crossland J, Stores R, et al. (2017) The impact of the physical home environment for family carers of people with dementia: A qualitative study. Journal of Housing for the Elderly 31: 303-333.
- Keller HH, Edward HG, Cook C (2007) Mealtime experiences of families with dementia. American Journal of Alzheimer's Disease & Other Dementias 21: 431-438.
- Gitlin LN, Winter L, Burke J, Chernett N, Dennis MP, et al. (2008) Tailored activities to manage neuropsychiatric behaviors in persons with dementia and reduce caregiver burden: A randomized pilot study. The American Journal of Geriatric Psychiatry 16: 229-239.
- Nomura M, Makimoto K, Kato M, Shiba T, Matsuura C, et al. (2009) Empowering older people with early dementia and family caregivers: A participatory action research study. International Journal of Nursing Studies 46: 431-441.
- O'Connor CM, Clemson L, Brodaty H, Gitlin LN, Piguet O, et al. (2016) Enhancing caregivers' understanding of dementia and tailoring activities in frontotemporal dementia: Two case study. Disability and Rehabilitation 38: 704-714.
- Caspi E (2014) Wayfinding difficulties among elders with dementia in an assisted living residence. Dementia 13: 429-450.
- Davis R, Ohman J (2016) Wayfinding in ageing and Alzheimer's disease within a virtual senior residence: Study protocol. Journal of Advanced Nursing 72: 1677-1688.
- Kessels RPC, van Doormaal A, Janzen G (2011) Landmark recognition in Alzheimer’s dementia: Spared implicit memory for objects relevant for navigation. PLoS ONE 6: e18611.
- Arntzen C, Holthe T, Jentoft R (2014) Tracing the successful incorporation of assistive technology into everyday life for younger people with dementia and family carers. Dementia 15: 646-662.
- Boger J, Quraishi M, Turcotte N, Dunal L (2014) The identification of assistive technologies being used to support the daily occupations of community-dwelling older adults with dementia: A cross-sectional pilot study. Disability and Rehabilitation: Assistive Technology 9: 17-30.
- Phinney A, Chaudhury H, O’Connor DL (2007) Doing as much as I can do: The meaning of activity for people with dementia. Aging and Mental Health 11: 384-393.
- Preston L, Marshall A, Bucks RS (2007) Investigating the ways that older people cope with dementia: A qualitative study. Aging & Mental Health 11: 131-143.
- Judge KS, Yarry SJ, Orsulic-Jeras S (2009) Acceptability and feasibility results of a strength-based skills training program for dementia caregiving dyads. The Gerontologist 50: 408-417.
- Cahill S, Begley E, Faulkner JP, Hagen I (2007) “It gives me a sense of independence”–Findings from Ireland on the use and usefulness of assistive technology for people with dementia. Technology and Disability 19: 133-142.
- Kurz A, Thöne-Otto A, Cramer B, Egert S, Frölich L, et al. (2012) CORDIAL: cognitive rehabilitation and cognitive-behavioral treatment for early dementia in Alzheimer disease: A multicenter, randomized, controlled trial. Alzheimer Disease & Associated Disorders 26: 246-253.
- Topo P, Saarikalle K, Begley E, Cahill S, Holthe T, et al. (2007) “I don't know about the past or the future, but today it's Friday” Evaluation of a time aid for people with dementia. Technology and Disability 19: 121-131.
- Kurz A, Pohl C, Ramsenthaler M, Sorg C (2009) Cognitive rehabilitation in patients with mild cognitive impairment. International Journal of Geriatric Psychiatry 24: 163-168.
- http://www.qualtrics.com
- Armstrong R, Kergoat H (2015) Oculo-visual changes and clinical considerations affecting older patients with dementia. Ophthalmic and Physiological Optics 35: 352-376.
- Lawrence V, Murray J, Ffytche D, Banerjee S (2009) “Out of sight, out of mind”: A qualitative study of visual impairment and dementia from three perspectives. International Psychogeriatrics 21: 511-518.
- Van Hoof J, Kort HSM (2009) Supportive living environments: A first concept of a dwelling designed for older adults with dementia. Dementia 8: 293-316.
- Regier NG, Hodgson NA, Gitlin LN (2016) Characteristics of activities for persons with dementia at the mild, moderate, and severe stages. The Gerontological Society of America 57: 987-997.
- Lindqvist E, Nygard L, Borell L (2013) Significant junctures on the way towards becoming a user of assistive technology in Alzheimer's disease. Scandinavian Journal of Occupational Therapy 20: 386-396.
Citation: Struckmeyer L, Killingsworth J, Hays S (2022) Visual Cues for Persons with Dementia: Opinions of Dementia Caregivers & Occupational Therapists. J Alzheimers Neurodegener Dis 8: 059.
Copyright: © 2022 Linda Struckmeyer, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.